
HEALTH BLOG
Ovarian Pain After Menopause: Understanding the Causes and Management
-
Rahul Priydarss
In this article, we will discuss the various factors that contribute to ovarian pain after menopause, including ovarian cysts, ovarian cancer, endometriosis, pelvic inflammatory disease (PID), adhesions or scar tissue, and hormonal changes.
What Is Menopause:
– Menopause is a natural biological process that occurs in women as they age, typically in their late 40s to early 50s, although the exact timing may vary from person to person. It marks the end of a woman’s reproductive years, marking the end of menstruation and a decline in the levels of reproductive hormones, particularly estrogen and progesterone, produced by the ovaries.
– Menopause is a natural and inevitable part of the aging process for women, usually occurring around the age of 51 on average. However, certain factors such as genetics, lifestyle, and underlying health conditions can influence the timing and experience of menopause for each woman.
– After menopause, women enter a new stage of life called postmenopause, during which they no longer menstruate and are no longer able to conceive naturally. While menopause marks the end of fertility, it does not signal the end of a woman’s overall health and well-being. With proper medical care and lifestyle adjustments, women can successfully recover from this infection and enjoy full and healthy lives after menopause.
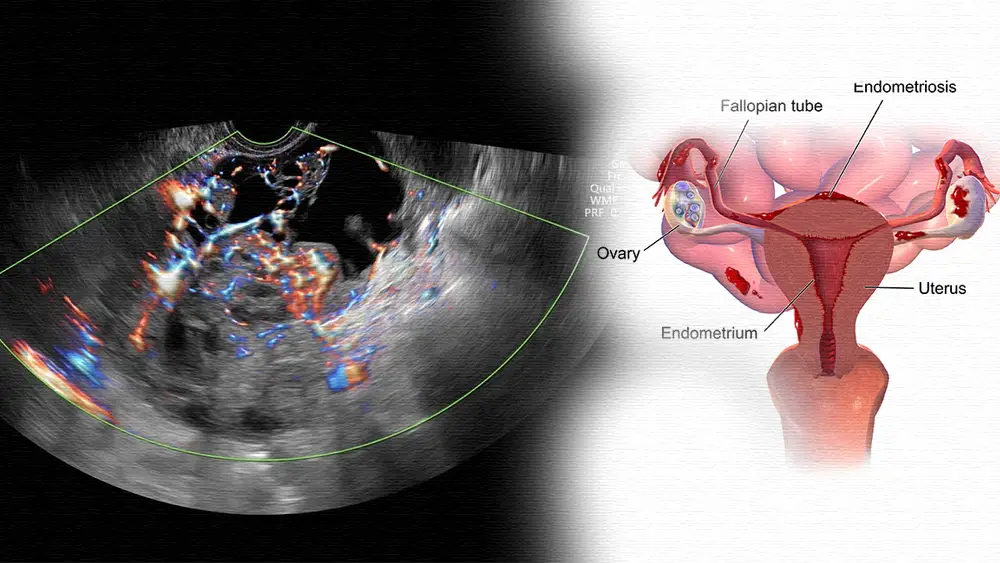
Table of Contents
– Ovarian pain is the pain you feel around your ovaries. If you have ovarian pain, you’ll probably feel it in your lower abdomen (below the navel), pelvis, or lower back. Sometimes, only one ovary hurts at a time. Other times, you may feel pain in both ovaries.
– Ovarian pain can be chronic or acute. Chronic pain is pain that occurs repeatedly and lasts for several months, while acute pain is pain that occurs suddenly and comes and goes.
– It is important to contact your healthcare provider if you have ovarian or pelvic pain. Several conditions can cause painful ovulation. Some may be serious, while others are mild. Getting to the underlying cause of pain determines treatment.
– Ovarian pain, also known as pelvic pain, refers to discomfort or tenderness experienced in the lower abdomen, specifically in the area of the ovaries. It is important to understand that ovarian pain can originate from a variety of sources, including the ovaries themselves or other surrounding organs in the pelvic area.
– The ovaries are two small, almond-shaped organs located on either side of the uterus, and they play an important role in the female reproductive system. Ovarian pain can occur for many reasons, and identifying the underlying cause is essential to determining appropriate treatment.
– Your ovaries are small, oval-shaped glands on either side of your uterus (a right ovary and a left ovary). They make and store your eggs, which you need to reproduce. Your ovaries also make hormones that trigger ovulation and menstruation.
Causes of Ovarian Pain After Menopause:
It is important for women experiencing persistent ovarian pain after menopause to consult a healthcare provider for thorough evaluation and appropriate management.
Ovarian cysts: Despite the end of the menstrual cycle, ovarian cysts can still develop in menopausal women. These fluid-filled sacs can form on the surface of the ovaries and can cause pain or discomfort if they burst or become larger.
Endometriosis: Women who have endometriosis may continue to experience pelvic pain after menopause. Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, often affecting the ovaries and causing pain.
Pelvic adhesions: Adhesions or scar tissue may develop in the pelvic area due to previous surgery or infection. These adhesions can cause organs to stick together, causing pelvic pain or discomfort.
Ovarian cancer: Although less common, ovarian cancer can also occur after menopause. Persistent pelvic pain can be a symptom of ovarian cancer, along with other symptoms such as bloating, abdominal swelling, and changes in bowel habits.
Pelvic inflammatory disease (PID): Infection of the female reproductive organs, including the ovaries, can cause pelvic pain even after menopause. PID is usually caused by a sexually transmitted infection or other bacterial infection.
Hormonal changes: Fluctuating hormone levels after menopause, especially estrogen, can also contribute to pelvic discomfort. Hormonal imbalance can affect the functioning of the reproductive organs and manifest as ovarian pain.
Urinary tract infection (UTI) or gastrointestinal problems: Pain in the pelvic area after menopause can sometimes be caused by urinary tract infection or gastrointestinal problems rather than being directly related to ovulation.

Symptoms of Ovarian Pain After Menopause:
It is important to note that these symptoms can vary in severity and duration from person to person.
Pelvic discomfort: Women may feel slight pain or pressure in the pelvic area. This discomfort may occur continuously or intermittently and vary in intensity.
Abdominal swelling: Some women may notice increased abdominal swelling or bloating, which may contribute to feelings of discomfort or fullness in the lower abdomen.
Pain during intercourse: Ovarian pain may increase during intercourse after menopause, causing discomfort or pain in the pelvic area.
Changes in bowel movements: Ovarian pain may be associated with changes in bowel movements, such as constipation or diarrhea. These changes may occur along with pelvic discomfort.
Nausea or vomiting: In some cases, women experiencing ovarian pain after menopause may also experience nausea or vomiting, especially if the pain is severe.
Urinary symptoms: Ovarian pain may be accompanied by urinary symptoms, such as increased frequency or urgency of urination, pain or burning during urination, or difficulty emptying the bladder.
Fatigue or weakness: Persistent ovarian pain after menopause can impact overall energy levels, causing feelings of fatigue or weakness.
Treatment Options for Ovarian Pain After Menopause:
In 2024 our medicine and doctors get many options for further menopause treatment.
Pain management: Over-the-counter pain relievers such as ibuprofen or acetaminophen can help relieve mild to moderate ovarian pain. Prescription medications may be prescribed for more severe pain, including nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids.
Hormonal therapy: Hormone replacement therapy (HRT) may be recommended to address hormonal imbalances that contribute to ovarian pain after menopause. Estrogen therapy may help reduce symptoms such as pelvic discomfort or vaginal dryness, although it may not be suitable for all women.
Surgical intervention: In cases where ovarian cysts are causing significant pain or discomfort, surgical removal of the cyst may be required. In some cases, hysterectomy or removal of the ovaries (oophorectomy) may be recommended to reduce symptoms, especially if ovarian cancer is suspected.
Medications for specific conditions: For women with endometriosis, medications such as hormonal contraceptives or gonadotropin-releasing hormone (GnRH) agonists may be prescribed to manage symptoms. Antibiotics may be prescribed to treat pelvic inflammatory disease (PID) if it is the underlying cause of ovarian pain.
Lifestyle changes: Maintaining a healthy diet rich in fruits, vegetables, and whole grains can help with overall pelvic health. Regular exercise can help reduce pelvic discomfort and improve overall health. Stress management techniques such as yoga, meditation or deep breathing exercises may help reduce ovarian pain associated with stress or anxiety.
Alternative treatments: Some women find relief from ovarian pain through alternative treatments such as acupuncture, chiropractic care, or herbal supplements. However, it is important to consult a healthcare provider before trying these methods.
Pelvic floor therapy: Pelvic floor physical therapy may be beneficial for women who experience pelvic pain after menopause, especially if the pain is related to muscle tension or weakness in the pelvic floor muscles.
Complementary therapy: Some women find relief from ovarian pain through complementary therapy methods such as massage therapy, aromatherapy, or hydrotherapy.
Psychological support: Counseling or therapy may be helpful for women experiencing chronic ovarian pain after menopause, especially if it is affecting their mental health or overall quality of life.
Regular follow-up: It is important for women undergoing treatment for ovarian pain after menopause to have regular follow-up appointments with their healthcare provider to monitor progress and adjust treatment as needed.
New Mathematical Model for Ovarian Tissue Cryopreservation:
- Using data from hundreds of past ovarian cryopreservation and transplantation procedures, and molecular studies of how ovarian follicles behave in ovarian tissue, Oktay and colleagues created a new mathematical model, published in the American Journal of Published in Obstetrics & Gynecology, to estimate how long the surgery will take. Menopause can be delayed in many circumstances in healthy women.
- A recently published mathematical model focusing on healthy women undergoing ovarian tissue cryopreservation takes into account several factors, including the age at which the patient receives the procedure, which can potentially affect how long into menopause. Delay may play an important role in this.
Menopause and Health Disadvantages in Females:
Menopause, a natural stage in a woman’s life marking the end of her reproductive years, can bring various health disadvantages. While menopause is a normal part of aging, the hormonal changes that occur during it can cause several health challenges for women. Here are some common health disadvantages associated with menopause-
Hot flashes and night sweats: Many women experience hot flashes and night sweats during menopause, which can disrupt sleep patterns and affect overall health.
Vaginal dryness and discomfort: Declining estrogen levels during menopause can cause vaginal dryness, itching, and discomfort, making intercourse painful or uncomfortable.
Bone loss and osteoporosis: Estrogen plays an important role in maintaining bone density, and declining estrogen levels during menopause can increase the risk of bone loss and osteoporosis, a condition in which bones become brittle and prone to fractures.
Risk of heart disease: The risk of heart disease increases significantly in women after menopause. Estrogen has a protective effect on the cardiovascular system, and its decline during menopause can increase the risk of heart disease and stroke.
Weight gain and changes in body composition: Many women experience changes in body composition during menopause, including weight gain, especially around the abdomen. This change in fat distribution may increase the risk of metabolic disorders such as diabetes and high blood pressure.
Mood changes and depression: Hormonal fluctuations during menopause may contribute to mood changes, irritability, and an increased risk of depression and anxiety in some women.
Sleep disturbances: Menopause symptoms such as hot flashes and night sweats can disrupt sleep patterns, leading to insomnia and daytime fatigue.
Urinary incontinence: Declining estrogen levels can cause the pelvic floor muscles to weaken, leading to urinary incontinence and bladder control problems in some women.
Sexual diseases: Changes in hormone levels and vaginal dryness can contribute to sexual dysfunction, including decreased libido and difficulty achieving orgasm, impacting sexual satisfaction and intimacy.
Cognitive Changes: Some women may experience cognitive changes during menopause, including difficulty concentrating, memory loss, and cognitive decline. However, more research is needed to fully understand the connection between menopause and cognitive function.
FAQs about Ovarian Pain After Menopause:
A1: Yes, ovarian pain can occur after menopause due to various factors such as ovarian cysts, endometriosis, or pelvic inflammatory disease.
A2: Symptoms may include pelvic discomfort, abdominal bloating, pain during intercourse, changes in bowel habits, and urinary symptoms.
A3: Diagnosis typically involves a physical examination, imaging tests such as ultrasound, blood tests, and sometimes laparoscopy to visualize the pelvic organs.
A4: Treatment may include pain management with medications, hormonal therapy, surgical intervention, lifestyle modifications, or alternative therapies.
A5: If you experience persistent or severe pelvic pain, changes in bowel or bladder habits, or other concerning symptoms, it’s essential to consult with a healthcare provider for evaluation and appropriate management.

-Please remember, to always consult with healthcare professionals or Doctors for personalised advice related to medical conditions.
Conclusion:
In conclusion, ovarian pain after menopause can be a challenging issue for many women. by understanding the causes, symptoms, diagnosis, treatment options, prevention strategies, and ways to live with the condition, women can take proactive steps to effectively manage their health and well-being.




