
HEALTH NEWS
Meningitis in Nigeria: Understanding the Threat, Mobilizing Solutions
-
Rahul Priydarss
Discover the Impact of Meningitis in Nigeria: Learn about the prevalence, recent outbreaks, and response efforts against this severe health concern. Explore the causes, transmission, and prevention methods, including vaccination campaigns and hygiene practices. Gain insights from the Nigeria Centre for Disease Control (NCDC) on addressing challenges and collaborating for enhanced surveillance and control. Stay informed about symptoms, diagnosis, treatment, and follow-up care to combat meningitis effectively. Empower yourself with knowledge and awareness to protect against this infectious disease in Nigeria.
Introduction to Nigeria Meningitis:
In Nigeria meningitis is a prevalent health concern, particularly during certain times of the year. The country experiences periodic outbreaks of meningitis, often during the dry season when environmental conditions are conducive to the spread of the disease. Nigeria’s geographical location in the African meningitis belt, coupled with factors such as overcrowded living conditions and limited access to healthcare, contributes to the high prevalence of meningitis in the country.
What is Meningitis:
Meningitis is a severe medical condition characterized by inflammation of the protective membranes covering the brain and spinal cord, known as the meninges. This inflammation is often caused by bacterial, viral, or fungal infections. When these pathogens invade the meninges, they trigger an immune response, leading to symptoms such as severe headache, fever, neck stiffness, nausea, vomiting, and sensitivity to light.
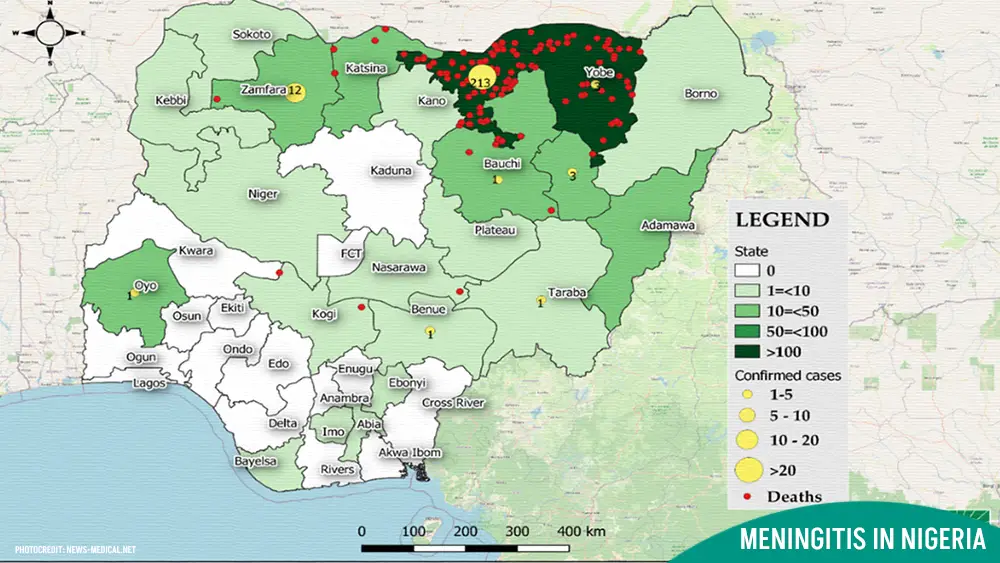
Table of Contents
What NCDC Says:
The Nigeria Centre for Disease Control (NCDC) says it is addressing multiple hurdles in its efforts to tackle epidemic-prone diseases in the country.
Dr Chikwe Ihekweazu, Director-General of NCDC, said this in an interview with the News Agency of Nigeria (NAN) on Tuesday in Abuja.
He said the agency was working tirelessly to tackle various challenges, including insufficient funding, inadequate healthcare infrastructure and resources, and vaccine hesitancy.
According to him, other challenges include limited surveillance systems for early detection and response, coordination gaps between government agencies and healthcare providers, and socioeconomic factors exacerbating vulnerability to disease outbreaks.
Ihekweazu disclosed that the NCDC was collaborating with state governments, international partners, and other stakeholders to strengthen disease surveillance, prevention, and control efforts across the country.
“We are working closely with state governments, international partners, and other stakeholders to enhance disease surveillance, early detection, and response to outbreaks.
The Prevalence of Meningitis in Nigeria:
In Nigeria, meningitis is a significant public health concern, with periodic outbreaks occurring throughout the country. These outbreaks often coincide with specific times of the year, particularly during the dry season when environmental conditions are conducive to the spread of the disease. Nigeria’s geographical location in the African meningitis belt further exacerbates the risk of meningitis transmission, making it a prevalent health issue in the region.
Recent Outbreaks of Meningitis in Nigeria:
In recent years, Nigeria has experienced several significant outbreaks of meningitis, underscoring the ongoing threat posed by this infectious disease. These outbreaks have resulted in considerable morbidity and mortality, particularly in regions with limited access to healthcare and vaccination services.
Notable Meningitis Outbreaks in Nigeria:
Nigeria has faced several notable meningitis outbreaks in recent years, highlighting the persistent threat posed by the disease. These outbreaks often occur in specific regions of the country and can vary in severity, resulting in significant morbidity and mortality among affected populations.
One such outbreak occurred in 2017, primarily affecting states in the northern region of Nigeria. The outbreak was attributed to the serogroup C strain of the meningitis bacteria, Neisseria meningitidis. Thousands of cases were reported, with a high number of fatalities recorded due to delays in diagnosis and treatment.
Another notable outbreak occurred in 2020, with several states in the northwest and north-central regions reporting a surge in meningitis cases. This outbreak, primarily caused by the serogroup A strain of Neisseria meningitidis, prompted swift response efforts from health authorities to contain the spread of the disease.
Response and Containment Efforts:
In response to meningitis outbreaks, health authorities in Nigeria implement various measures to contain the spread of the disease and mitigate its impact on affected communities. These efforts typically include.
Vaccination Campaigns: Health authorities conduct targeted vaccination campaigns in areas experiencing meningitis outbreaks. Vaccination helps build immunity against specific strains of the meningitis bacteria, reducing the risk of transmission and protecting vulnerable populations.
Surveillance and Early Detection: Surveillance systems are strengthened to monitor the incidence of meningitis cases and detect outbreaks promptly. Early detection allows for swift intervention and the implementation of control measures to prevent further spread.
Treatment and Care: Healthcare facilities are equipped to provide prompt diagnosis and treatment of meningitis cases. Antibiotics are administered to individuals diagnosed with bacterial meningitis, while supportive care measures are implemented to manage symptoms and prevent complications.
Public Awareness Campaigns: Health authorities conduct public awareness campaigns to educate communities about meningitis symptoms, prevention strategies, and the importance of seeking medical attention promptly. These campaigns aim to dispel myths and misconceptions surrounding the disease, encouraging early detection and treatment.
Collaboration with International Partners: Nigeria collaborates with international partners and organizations, such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), to access technical expertise, resources, and support for meningitis control efforts. These partnerships facilitate the exchange of information and best practices, strengthening Nigeria’s capacity to respond effectively to meningitis outbreaks.
Causes and Transmission of Meningitis:
Meningitis can be caused by various pathogens, including bacteria, viruses, and fungi. Each type of meningitis has its distinct causes and modes of transmission.
Bacterial Meningitis: Bacterial meningitis is often caused by certain bacteria, with the most common culprits being Neisseria meningitidis, Streptococcus pneumonia, and Haemophilus influenzae type b (Hib). These bacteria can spread through respiratory droplets when an infected person coughs or sneezes, leading to transmission to others nearby.
Bacterial meningitis can also occur when bacteria from infections in other parts of the body, such as the ears or sinuses, spread through the bloodstream to the meninges. Certain factors, such as crowded living conditions, close contact with an infected individual, or a weakened immune system, can increase the risk of bacterial meningitis transmission.
Viral Meningitis: Viral meningitis is typically caused by common viruses, including enteroviruses, herpes simplex virus, and varicella-zoster virus. These viruses are often spread through respiratory secretions, fecal-oral transmission, or direct contact with an infected person. Viral meningitis is usually less severe than bacterial meningitis and often resolves on its own with supportive care.
While viral meningitis is contagious, the risk of transmission is generally lower compared to bacterial meningitis. However, outbreaks can occur in settings where people are in close contact with one another, such as schools, dormitories, or healthcare facilities.
Fungal Meningitis: Fungal meningitis is less common than bacterial or viral meningitis and is usually caused by fungal pathogens such as Cryptococcus neoforman or Candida species. Fungal meningitis typically occurs in individuals with compromised immune systems, such as those with HIV/AIDS, cancer, or diabetes, or those taking immunosuppressive medications.
Fungal meningitis can result from inhaling fungal spores from the environment or the dissemination of fungal infections from other parts of the body. Unlike bacterial and viral meningitis, fungal meningitis is not transmitted from person to person.
Signs and Symptoms of Meningitis:
Meningitis presents with a variety of signs and symptoms, which can vary depending on the cause and severity of the infection. Prompt recognition of these symptoms is crucial for early diagnosis and treatment.
Fever and Headache: Fever and headache are hallmark symptoms of meningitis. The fever may develop suddenly and be accompanied by chills. The headache associated with meningitis is often severe and persistent, and it may worsen over time. Individuals with meningitis may describe the headache as intense and throbbing, making it difficult to perform daily activities.
Neck Stiffness: Neck stiffness, also known as nuchal rigidity, is another common symptom of meningitis. This stiffness occurs due to inflammation of the meninges, which causes discomfort and limited movement of the neck. When attempting to touch the chin to the chest, individuals with meningitis may experience resistance and pain in the neck muscles.
Sensitivity to Light: Sensitivity to light, medically referred to as photophobia, is a characteristic symptom of meningitis. Individuals with meningitis may find bright lights uncomfortable or even painful, leading them to avoid exposure to light. Photophobia can exacerbate the headache and neck stiffness experienced by individuals with meningitis, further contributing to their discomfort.
Other Symptoms: In addition to fever, headache, neck stiffness, and sensitivity to light, meningitis can cause a range of other symptoms, including.
- Nausea and vomiting
- Altered mental status or confusion
- Drowsiness or lethargy
- Seizures
- Skin rash (in certain types of meningitis, such as meningococcal meningitis)
It’s important to note that the onset of symptoms can be rapid, and they may progress quickly, particularly in cases of bacterial meningitis. Therefore, any individual experiencing symptoms suggestive of meningitis should seek immediate medical attention for evaluation and treatment.

Diagnosis and Treatment of Meningitis:
Meningitis requires prompt diagnosis and treatment to prevent serious complications and reduce the risk of mortality. Healthcare providers use a combination of diagnostic tests and therapeutic interventions to manage meningitis effectively.
Lumbar Puncture: Lumbar puncture, also known as a spinal tap, is a crucial diagnostic procedure used to confirm the diagnosis of meningitis. During a lumbar puncture, a healthcare provider inserts a needle into the lower part of the spine to collect cerebrospinal fluid (CSF), which surrounds the brain and spinal cord. Analysis of the CSF can reveal the presence of pathogens, such as bacteria, viruses, or fungi, as well as abnormal levels of white blood cells and proteins, indicative of inflammation.
Antibiotics and Antiviral Drugs: The choice of treatment for meningitis depends on the underlying cause of the infection. For bacterial meningitis, antibiotics are the mainstay of treatment. Empirical antibiotic therapy is initiated immediately upon suspicion of bacterial meningitis, pending the results of CSF analysis. Commonly used antibiotics for bacterial meningitis include third-generation cephalosporins (e.g., ceftriaxone or cefotaxime) and vancomycin. Once the causative pathogen is identified and susceptibility testing is performed, antibiotic therapy may be adjusted accordingly.
In cases of viral meningitis, antiviral drugs may be prescribed if the infection is caused by herpes simplex virus or varicella-zoster virus. Antiviral medications, such as acyclovir or ganciclovir, can help reduce the severity and duration of symptoms and prevent complications.
Supportive Care: Supportive care is an essential component of meningitis treatment, aimed at relieving symptoms, maintaining hydration, and preventing complications. Supportive measures may include:
- Pain management: Analgesic medications, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate headache and fever associated with meningitis.
- Fluid and electrolyte balance: Intravenous fluids may be administered to maintain hydration and electrolyte balance, particularly in individuals with severe symptoms or complications such as dehydration or electrolyte imbalances.
- Monitoring and observation: Close monitoring of vital signs, neurological status, and response to treatment is necessary to assess the patient’s condition and adjust therapy as needed.
Follow-Up and Monitoring: Following initial treatment, patients with meningitis require close follow-up and monitoring to evaluate their response to therapy and detect any complications. Repeat lumbar puncture and CSF analysis may be performed to assess the effectiveness of treatment and ensure the resolution of inflammation. Additionally, patients may require ongoing medical care, rehabilitation, and support services to manage any long-term sequelae of meningitis, such as neurological deficits or cognitive impairment.
Prevention and Control of Meningitis:
Preventing meningitis requires a combination of vaccination and good hygiene practices to reduce the risk of infection and transmission of the disease. Preventing meningitis transmission requires a combination of vaccination, good hygiene practices, and prompt treatment of infections. Vaccination against bacterial pathogens such as Neisseria meningitidis, Streptococcus pneumonia, and Haemophilus influenzae type b can significantly reduce the risk of bacterial meningitis.
Practicing good respiratory hygiene, such as covering coughs and sneezes, and maintaining proper hand hygiene can help prevent the spread of respiratory viruses that can cause viral meningitis. Additionally, avoiding close contact with individuals who are sick and practicing safe sex can reduce the risk of certain viral infections that can lead to meningitis.
While fungal meningitis is less common, individuals at higher risk should take precautions to minimize exposure to fungal pathogens, such as avoiding environments where fungal spores may be present and seeking prompt medical attention for any signs of infection.
Vaccination:
Vaccination is the most effective way to prevent certain types of bacterial meningitis, such as those caused by Neisseria meningitidis, Streptococcus pneumonia, and Haemophilus influenzae type b (Hib). Vaccines against these pathogens stimulate the body’s immune response, providing immunity against meningitis-causing bacteria.
Recommended Vaccines:
Vaccination recommendations may vary by age, health status, and risk factors. It’s essential to follow the vaccination schedule recommended by healthcare providers and public health authorities to ensure optimal protection against meningitis.
- Meningococcal vaccine: Protects against meningococcal meningitis caused by Neisseria meningitidis. Different types of meningococcal vaccines are available, including conjugate vaccines and serogroup-specific vaccines.
- Pneumococcal vaccine: Prevents pneumococcal meningitis caused by Streptococcus pneumonia. The pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) are recommended for different age groups and risk factors.
- Haemophilus influenzae type b (Hib) vaccine: Protects against Hib meningitis. The Hib vaccine is part of routine childhood immunization schedules in many countries.
Hygiene Practices:
Good hygiene practices can help reduce the risk of meningitis transmission, particularly viral and fungal meningitis, which may spread through respiratory secretions or direct contact with an infected person. Key hygiene measures include:
- Handwashing: Washing hands frequently with soap and water for at least 20 seconds helps remove pathogens from the hands and prevents their transmission to the mouth, nose, or eyes.
- Respiratory etiquette: Covering coughs and sneezes with a tissue or the elbow, rather than hands, can help prevent the spread of respiratory droplets containing infectious agents.
- Avoiding close contact with sick individuals: Minimizing close contact with individuals who have respiratory infections or symptoms of meningitis can reduce the risk of transmission.
- Maintaining a clean environment: Regular cleaning and disinfection of frequently touched surfaces, such as doorknobs, light switches, and shared objects, can help prevent the spread of pathogens that cause meningitis.
Awareness and Education Initiatives regarding Meningitis:
Raising awareness about meningitis and educating communities about prevention strategies are essential components of public health efforts to combat the disease. Various initiatives, including government campaigns and community outreach programs, play a vital role in disseminating information and promoting proactive measures to prevent meningitis.
Government Campaigns:
Government-led campaigns are instrumental in reaching large segments of the population and raising awareness about meningitis. These campaigns often utilize multiple channels, including mass media, social media, and community events, to disseminate information about the signs and symptoms of meningitis, vaccination recommendations, and the importance of seeking medical care promptly.
Government campaigns may include:
- Public Service Announcements (PSAs): Broadcast on television, radio, and online platforms, PSAs deliver concise messages about meningitis prevention and the availability of vaccines.
- Educational Materials: Government health agencies produce informational brochures, posters, and fact sheets that provide detailed guidance on recognizing the signs of meningitis and taking appropriate preventive measures.
- Vaccination Drives: Governments organize vaccination drives targeting high-risk populations, such as children, adolescents, and young adults, to increase vaccine coverage and protect against meningitis outbreaks.
- School-Based Programs: Educational initiatives implemented in schools raise awareness among students, teachers, and parents about meningitis symptoms, prevention strategies, and the importance of vaccination.
Community Outreach Programs: Community outreach programs play a crucial role in engaging local communities, addressing cultural beliefs and practices, and promoting behavior change related to meningitis prevention. These programs are often implemented by local health authorities, non-governmental organizations (NGOs), and community-based organizations (CBOs) with strong ties to the community.
Community outreach programs may involve:
- Health Education Workshops: Conducted in community centers, religious institutions, and other gathering places, health education workshops provide interactive sessions on meningitis prevention, hygiene practices, and vaccination.
- Door-to-Door Campaigns: Volunteers and healthcare workers go door-to-door in neighborhoods to distribute informational materials, engage residents in conversations about meningitis, and provide guidance on accessing healthcare services.
- Mobile Clinics: Mobile clinics visit underserved areas to offer free or low-cost vaccinations, health screenings, and consultations with healthcare providers. These clinics increase access to preventive care and promote early detection of meningitis cases.
- Community Events: Health fairs, festivals, and community events provide opportunities to disseminate information about meningitis in a festive and engaging environment. Booths, exhibits, and interactive activities raise awareness and encourage participation in preventive measures.
FAQs about Nigeria Meningitis:
A1: Common symptoms of meningitis include severe headache, fever, neck stiffness, nausea, vomiting, and sensitivity to light.
A2: Meningitis is diagnosed through a combination of clinical evaluation and laboratory tests, including cerebrospinal fluid analysis and imaging studies.
A3: Treatment for meningitis typically involves antibiotic therapy for bacterial meningitis and antiviral or antifungal medications for viral or fungal meningitis, respectively.
A4: Vaccination programs targeting high-risk populations and public health measures such as promoting hygiene and sanitation can help prevent meningitis outbreaks.
A5: Nigeria faces challenges such as limited healthcare infrastructure, inadequate access to healthcare services, and socioeconomic disparities in combating meningitis effectively.

-Please remember, to always consult with healthcare professionals or Doctors for personalized advice related to medical conditions.
Conclusion:
In conclusion, meningitis remains a significant public health challenge in Nigeria, with periodic outbreaks posing risks to the population’s health and well-being. Understanding the epidemiology, risk factors, symptoms, and prevention strategies is essential for effectively combating meningitis in the country. By implementing comprehensive and integrated approaches, Nigeria can reduce the incidence of meningitis and mitigate its impact on individuals and communities.





thanks.
hello