
NEUROSCIENCE
What is Brain Stroke, Symptoms, Causes, Types and Treatment
-
Rahul Priydarss
Discover everything you need to know about Brain Stroke in this comprehensive article. From understanding the causes and symptoms to exploring treatment options and prevention strategies, this guide provides invaluable insights into recognizing, responding to, and recovering from strokes. Whether you’re seeking information for yourself or a loved one, this resource equips you with the knowledge to navigate this critical medical condition with confidence.
Introduction to Brain Stroke:
Brain stroke, also known simply as a stroke, is a critical medical emergency that occurs when there is a disruption in the blood supply to the brain. This interruption deprives the brain of essential oxygen and nutrients, leading to damage or death of brain cells within minutes. Strokes can have severe and often lasting effects on various bodily functions, including movement, speech, and cognition.
Strokes can occur suddenly and without warning, making them a leading cause of disability and mortality worldwide. Understanding the causes, symptoms, and immediate actions to take during a stroke is crucial for minimizing damage and improving outcomes.
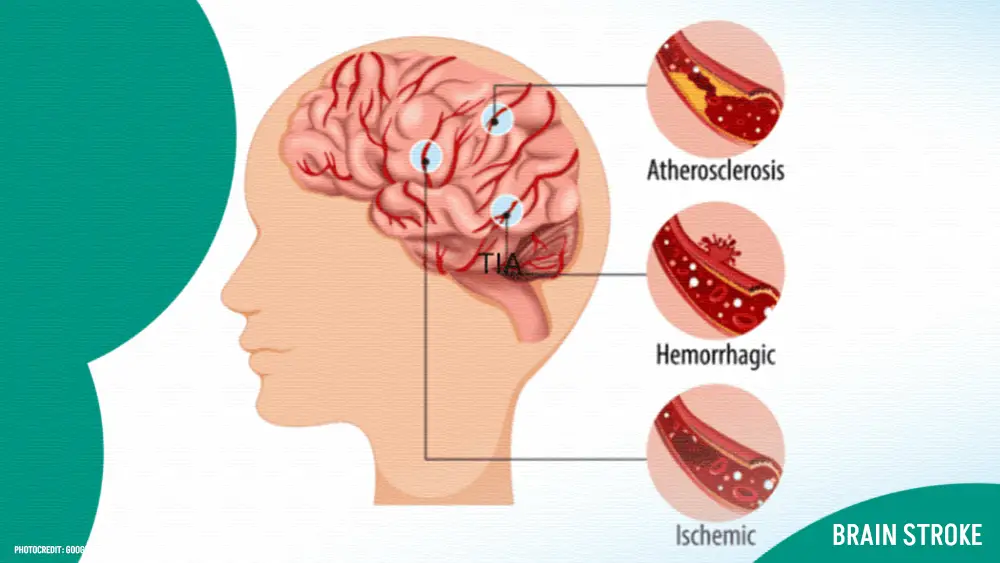
Table of Contents
Understanding Brain Stroke:
Brain stroke, or simply stroke, is a critical medical condition characterized by a disruption in the blood supply to the brain. This interruption results in damage to brain cells due to a lack of oxygen and nutrients. Understanding the causes and types of brain stroke is essential for prevention, early detection, and effective treatment.
Causes of Brain Stroke:
Blood Clots: One of the most common causes of stroke is the formation of blood clots within blood vessels supplying the brain. These clots can block or restrict blood flow to parts of the brain, leading to ischemic stroke.
Atherosclerosis: The buildup of plaque within arteries, a condition known as atherosclerosis, can narrow the blood vessels and impede blood flow to the brain, increasing the risk of stroke.
High Blood Pressure: Hypertension is a significant risk factor for stroke. Elevated blood pressure can weaken blood vessels over time, making them more susceptible to rupture and hemorrhagic stroke.
Heart Conditions: Certain heart conditions, such as atrial fibrillation, heart valve defects, and heart attacks, can contribute to the formation of blood clots that may travel to the brain and cause a stroke.
Diabetes: Individuals with diabetes are at higher risk of developing atherosclerosis and hypertension, both of which are major contributors to stroke risk.
Smoking: Tobacco smoke contains harmful chemicals that can damage blood vessels and promote the formation of blood clots, increasing the likelihood of stroke.
Obesity: Being overweight or obese is associated with various risk factors for stroke, including high blood pressure, diabetes, and unhealthy cholesterol levels.
High Cholesterol: Elevated levels of cholesterol in the blood can lead to the buildup of plaque within arteries, narrowing the blood vessels and predisposing individuals to stroke.
Types of Brain Stroke:
Brain stroke, a serious medical emergency, manifests in two primary types: ischemic stroke and hemorrhagic stroke. Understanding these types, their characteristics, and implications is crucial for effective management and treatment.
1. Ischemic Stroke:
Ischemic stroke, accounting for approximately 85% of all stroke cases, occurs when a blood clot or plaque buildup obstructs a blood vessel supplying blood to the brain. This blockage deprives brain tissue of oxygen and vital nutrients, leading to cellular damage and dysfunction. Ischemic strokes can be further categorized into two subtypes.
A. Thrombotic Stroke:
Definition: This type of ischemic stroke occurs when a blood clot forms within one of the arteries supplying blood to the brain.
Causes: Atherosclerosis, a condition characterized by the buildup of plaque within arteries, is a common cause of thrombotic strokes.
Risk Factors: Hypertension, diabetes, smoking, and high cholesterol levels increase the risk of thrombotic strokes.
Treatment: Treatment may involve administering clot-busting medications (thrombolytics) or performing a mechanical thrombectomy to remove the clot and restore blood flow to the brain.
B. Embolic Stroke:
Definition: Embolic strokes occur when a blood clot or other debris, known as an embolus, travels from another part of the body and lodges in a blood vessel supplying the brain.
Causes: Atrial fibrillation, heart valve defects, and blood clots originating from the heart are common sources of emboli.
Risk Factors: Individuals with heart conditions or a history of blood clots are at increased risk of experiencing embolic strokes.
Treatment: Similar to thrombotic strokes, treatment may involve thrombolytic therapy or mechanical thrombectomy to remove the embolus and restore blood flow.
2. Hemorrhagic Stroke:
Hemorrhagic stroke occurs when a weakened blood vessel ruptures, causing bleeding into the brain or the spaces surrounding it. This bleeding can exert pressure on brain tissue, leading to neurological deficits and potentially life-threatening complications. Hemorrhagic strokes are classified into two main types.
A. Intracerebral Hemorrhage:
Definition: Intracerebral hemorrhage occurs when a blood vessel within the brain ruptures and leaks blood into the surrounding brain tissue.
Causes: Chronic hypertension, cerebral amyloid angiopathy, and arteriovenous malformations are common causes of intracerebral hemorrhage.
Symptoms: Symptoms may include sudden severe headache, weakness or numbness on one side of the body, and altered consciousness.
Treatment: Treatment aims to control bleeding, reduce intracranial pressure, and stabilize vital signs. Surgical interventions may be necessary in some cases.
B. Subarachnoid Hemorrhage:
Definition: Subarachnoid hemorrhage occurs when there is bleeding into the space between the brain and the surrounding membranes (subarachnoid space).
Causes: Ruptured cerebral aneurysms, trauma, and arteriovenous malformations are common causes of subarachnoid hemorrhage.
Symptoms: Symptoms may include sudden severe headache (often described as the worst headache of one’s life), nausea, vomiting, and altered mental status.
Treatment: Treatment involves controlling bleeding, preventing complications such as vasospasm, and addressing the underlying cause of the hemorrhage through surgical or endovascular procedures.
Symptoms of Brain Stroke:
Brain stroke, also known as a cerebrovascular accident (CVA), can manifest with various symptoms, depending on the type of stroke and the specific area of the brain affected. Recognizing these symptoms is crucial for prompt medical intervention and optimising outcomes. Common symptoms of brain stroke include.
Common Symptoms:
When it comes to identifying a brain stroke, there are several common symptoms to watch out for. These include.
Sudden numbness or weakness: This often affects one side of the body, typically the face, arm, or leg. It can manifest as a sudden loss of sensation or strength.
Difficulty speaking or understanding: A person experiencing a stroke may have trouble speaking clearly or understanding speech. They may slur their words or find it challenging to comprehend what others are saying.
Confusion: Stroke can cause sudden confusion or disorientation. The individual may have trouble understanding their surroundings or following simple instructions.
Trouble walking or maintaining balance: Coordination and balance may be compromised during a stroke, leading to dizziness, stumbling, or difficulty walking.
Sudden severe headache: A sudden and intense headache, often described as the worst headache of one’s life, can indicate a stroke, especially when it occurs abruptly without any apparent cause.
Signs of Stroke in Women:
In addition to the common symptoms, women may experience certain signs that are more specific to them during a stroke.
Fainting or loss of consciousness: Women may faint or lose consciousness during a stroke, which can be a sign of reduced blood flow to the brain.
Hiccups: Persistent hiccups, particularly if they occur suddenly and are unrelated to eating or drinking, can be a warning sign of a stroke in women.
Nausea or vomiting: Some women may experience nausea, vomiting, or sudden onset of gastrointestinal symptoms during a stroke, which may be mistaken for other conditions.
General weakness: A feeling of overall weakness or fatigue, especially when it comes on suddenly and is accompanied by other stroke symptoms, should not be ignored, particularly in women.
Shortness of breath: Difficulty breathing or sudden shortness of breath can occur during a stroke, especially if it is caused by a blood clot in the lungs or other complications.
Immediate Actions During a Brain Stroke:
When it comes to a brain stroke, time is of the essence. Taking immediate action can significantly impact the outcome and reduce the risk of long-term complications. Here are the key steps to take.
FAST: Recognizing Stroke Symptoms:
When it comes to responding to a potential brain stroke, it’s crucial to act swiftly. One effective way to recognize stroke symptoms is to remember the acronym FAST.
- Face drooping: Ask the person to smile. Does one side of their face droop or seem uneven?
- Arm weakness: Ask the person to raise both arms. Does one arm drift downward, or is there weakness on one side?
- Speech difficulty: Ask the person to repeat a simple phrase. Is their speech slurred or difficult to understand?
- Time to call emergency services: If you observe any of these signs, it’s time to call for help immediately. Time is of the essence when it comes to treating a stroke.
Recognizing these symptoms and taking swift action can significantly improve the chances of survival and reduce the risk of long-term disability. Every minute counts, so don’t hesitate to call emergency services if you suspect someone is having a stroke.
Importance of Quick Action:
The importance of quick action cannot be overstated when it comes to responding to a brain stroke. Time is critical, as prompt medical intervention can help minimize brain damage and improve outcomes.
Minimizing brain damage: During a stroke, brain cells are deprived of oxygen and nutrients, leading to irreversible damage if left untreated. Acting quickly can help limit the extent of brain injury and preserve vital functions.
Administering timely treatment: Certain treatments, such as clot-busting medications or mechanical thrombectomy, are most effective when administered within a narrow window of time. Delaying medical care can reduce the effectiveness of these interventions and worsen the prognosis.
Improving chances of recovery: Early intervention not only reduces the severity of disability but also enhances the likelihood of recovery. Rehabilitation efforts are more effective when initiated early, helping stroke survivors regain lost skills and independence.
Treatment Options for Brain Stroke:
When someone experiences a brain stroke, prompt medical intervention is crucial to minimize damage to the brain and improve outcomes. The treatment options for brain stroke may vary depending on the type of stroke and its severity. Here are some common treatment approaches.
Emergency Medical Treatment:
Clot-busting medications (Thrombolytics): For ischemic strokes, which occur due to a blockage in a blood vessel, clot-busting drugs such as tissue plasminogen activator (tPA) may be administered intravenously to dissolve the clot and restore blood flow to the brain. These medications are most effective when given within a few hours of the onset of symptoms.
Mechanical thrombectomy: In some cases of large artery occlusion ischemic strokes, a procedure known as mechanical thrombectomy may be performed. This involves the insertion of a catheter into the blocked blood vessel to remove the clot mechanically, restoring blood flow to the brain.
Medication to prevent further complications: After the acute phase of a stroke, medications such as antiplatelet drugs (e.g., aspirin, clopidogrel) or anticoagulants (e.g., warfarin, dabigatran) may be prescribed to prevent blood clots and reduce the risk of recurrent strokes.
Rehabilitation and Recovery:
Physical therapy: Physical therapy focuses on improving mobility, strength, and coordination. It may include exercises to strengthen muscles, improve balance, and regain motor skills lost due to the stroke.
Occupational therapy: Occupational therapists help stroke survivors relearn daily activities such as eating, dressing, and bathing. They may provide adaptive equipment and techniques to facilitate independence and improve quality of life.
Speech therapy: Speech therapists work with individuals who have difficulty speaking, understanding language, or swallowing due to a stroke. They use exercises and techniques to improve communication skills and address swallowing difficulties.
Cognitive rehabilitation: Cognitive rehabilitation focuses on improving cognitive functions such as memory, attention, and problem-solving skills. It may include memory exercises, cognitive training programs, and strategies to compensate for cognitive deficits.
Surgical Interventions:
Surgery to repair aneurysms: In cases of hemorrhagic strokes caused by a ruptured aneurysm, surgery may be necessary to repair the weakened blood vessel and prevent further bleeding.
Surgical clipping or coiling: For cerebral aneurysms, surgical clipping or endovascular coiling may be performed to prevent rupture and reduce the risk of recurrent hemorrhagic strokes.
Preventing Brain Stroke:
While some risk factors for brain stroke, such as age and family history, cannot be changed, there are several lifestyle modifications and medical interventions that can help reduce the risk of experiencing a stroke. Here are some key strategies for stroke prevention:
Lifestyle Changes:
Manage high blood pressure: High blood pressure is the single most important risk factor for stroke. Monitoring blood pressure regularly and taking medications as prescribed by a healthcare provider can help control hypertension and reduce the risk of stroke.
Control diabetes: Individuals with diabetes are at increased risk of stroke. Keeping blood sugar levels under control through diet, exercise, medication, and regular monitoring can help prevent stroke and other complications associated with diabetes.
Maintain a healthy weight: Obesity and being overweight are risk factors for stroke. Adopting a healthy diet rich in fruits, vegetables, whole grains, and lean proteins, along with regular physical activity, can help maintain a healthy weight and reduce the risk of stroke.
Quit smoking: Smoking significantly increases the risk of stroke by damaging blood vessels and promoting the formation of blood clots. Quitting smoking and avoiding exposure to secondhand smoke can greatly reduce the risk of stroke and improve overall cardiovascular health.
Limit alcohol consumption: Excessive alcohol consumption can raise blood pressure and increase the risk of stroke. Limiting alcohol intake to moderate levels (no more than one drink per day for women and two drinks per day for men) can help reduce the risk of stroke.
Exercise regularly: Regular physical activity can help lower blood pressure, improve cholesterol levels, and maintain a healthy weight, all of which contribute to reducing the risk of stroke. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week.
Medical Interventions:
Take medications as prescribed: Medications such as antiplatelet drugs (e.g., aspirin, clopidogrel) or anticoagulants (e.g., warfarin, dabigatran) may be prescribed to prevent blood clots and reduce the risk of stroke, particularly for individuals with certain medical conditions such as atrial fibrillation or a history of stroke.
Manage cholesterol levels: High cholesterol levels can lead to atherosclerosis, a narrowing of the arteries that can increase the risk of stroke. Medications such as statins may be prescribed to lower cholesterol levels and reduce the risk of stroke.
Treat atrial fibrillation: Atrial fibrillation (an irregular heartbeat) is a significant risk factor for stroke. Treating atrial fibrillation with medications or procedures such as catheter ablation can help reduce the risk of blood clots and stroke.
Control other medical conditions: Managing other medical conditions such as heart disease, peripheral artery disease, and sleep apnea can help reduce the risk of stroke and improve overall cardiovascular health.
Other Preventive Measures:
Eat a healthy diet: A diet rich in fruits, vegetables, whole grains, and lean proteins can help lower blood pressure, cholesterol levels, and the risk of stroke. Limiting salt, saturated fats, and trans fats in the diet is also important for stroke prevention.
Stay hydrated: Drinking an adequate amount of water each day can help prevent dehydration, which can increase the risk of stroke. Aim to drink at least eight glasses of water per day, or more if you’re physically active or in hot weather.
Manage stress: Chronic stress can contribute to high blood pressure and other risk factors for stroke. Finding healthy ways to manage stress, such as relaxation techniques, exercise, and social support, can help reduce the risk of stroke.
Recovery and Rehabilitation:
Recovery from a brain stroke often involves a comprehensive rehabilitation program tailored to the individual’s needs. This may include physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation. Here are two key components of the recovery and rehabilitation process.
Physical Therapy:
Physical therapy plays a crucial role in helping stroke survivors regain mobility, strength, and independence. A physical therapist works closely with the individual to develop a personalized exercise program that addresses specific impairments and goals. Here’s how physical therapy can benefit stroke survivors.
Improving mobility: Physical therapists use a variety of techniques and exercises to help stroke survivors regain the ability to walk, stand, and move independently. This may include strength training, balance exercises, and gait training.
Rehabilitating affected limbs: Stroke can cause weakness or paralysis in one side of the body (hemiparesis). Physical therapy focuses on strengthening and retraining the affected limbs through exercises and activities designed to improve motor function and coordination.
Preventing complications: Immobility and muscle weakness can increase the risk of complications such as muscle contractures, pressure ulcers, and venous thrombosis. Physical therapy helps prevent these complications by promoting movement, proper positioning, and skin care.
Assisting with adaptive devices: Physical therapists may recommend and teach the use of assistive devices such as canes, walkers, and wheelchairs to improve mobility and safety.
Providing education and support: Physical therapists educate stroke survivors and their caregivers about proper body mechanics, fall prevention strategies, and exercises to continue at home. They also offer emotional support and encouragement throughout the recovery process.
Cognitive Rehabilitation:
Cognitive rehabilitation focuses on improving cognitive functions such as memory, attention, problem-solving, and executive functioning following a brain stroke. Cognitive deficits are common after stroke, but with targeted interventions, many individuals can regain or improve cognitive abilities. Here’s how cognitive rehabilitation can help.
Assessment and goal setting: Cognitive rehabilitation begins with a comprehensive assessment of cognitive strengths and weaknesses. Based on the assessment results, specific goals are established to target areas of difficulty.
Cognitive exercises and strategies: Cognitive rehabilitation programs include a variety of exercises and strategies designed to improve cognitive skills. These may include memory exercises, attention-training tasks, problem-solving activities, and use of compensatory strategies.
Functional training: Cognitive rehabilitation focuses on improving cognitive skills in the context of everyday activities and tasks. Stroke survivors practice cognitive skills in real-life situations to promote generalization and transfer of learning.
Adaptive techniques and technologies: Cognitive rehabilitation may involve teaching stroke survivors how to use assistive technologies and adaptive strategies to compensate for cognitive deficits. This may include memory aids, calendars, smartphone apps, and other tools.
Support and encouragement: Cognitive rehabilitation is a collaborative process that involves support from therapists, caregivers, and peers. Therapists provide encouragement, feedback, and guidance throughout the rehabilitation process to help stroke survivors achieve their cognitive goals.
Long-Term Outlook and Prognosis:
After experiencing a brain stroke, individuals and their families often wonder about the long-term implications and prognosis. While every case is unique and recovery varies depending on several factors, including the severity of the stroke and the individual’s overall health, understanding the long-term outlook can provide valuable insight. Here are some considerations regarding the long-term prognosis after a brain stroke.
Factors Affecting Recovery:
Severity of the stroke: The extent of brain damage caused by the stroke significantly impacts the long-term prognosis. Severe strokes may result in more profound and lasting impairments, while milder strokes may lead to better recovery outcomes.
Location of the stroke: The area of the brain affected by the stroke determines the specific functions that may be impaired. Damage to critical areas responsible for motor control, speech, or cognition can have significant implications for long-term functioning and independence.
Pre-existing health conditions: The presence of other medical conditions, such as diabetes, heart disease, or prior strokes, can influence the long-term prognosis. Managing underlying health issues and adopting a healthy lifestyle can positively impact recovery and overall well-being.
Age and overall health: Younger individuals and those in good overall health tend to have better recovery outcomes compared to older adults or those with multiple health problems. However, improvements in medical care and rehabilitation have made significant strides in enhancing outcomes for stroke survivors of all ages.
Access to rehabilitation: The availability and intensity of rehabilitation services play a crucial role in long-term recovery. Access to comprehensive rehabilitation programs, including physical therapy, occupational therapy, and speech therapy, can significantly improve functional outcomes and quality of life.
Adjusting to Life After Stroke:
While the road to recovery may be challenging, many stroke survivors adapt to their new circumstances and lead fulfilling lives. Here are some key aspects of adjusting to life after a stroke.
Setting realistic goals: Setting achievable goals, both short-term and long-term, can provide motivation and direction during the recovery process. Celebrating milestones, no matter how small, helps maintain a positive outlook.
Seeking support: Building a support network of family, friends, healthcare professionals, and support groups can provide valuable emotional support, practical assistance, and information-sharing opportunities.
Embracing assistive devices: Utilizing assistive devices and technologies, such as mobility aids, communication devices, and home modifications, can enhance independence and facilitate participation in daily activities.
Maintaining a healthy lifestyle: Adopting healthy habits, including regular exercise, nutritious diet, adequate sleep, and stress management, promotes overall well-being and may reduce the risk of recurrent strokes and other health complications.
Prognosis and Hope:
While the long-term prognosis after a brain stroke varies for each individual, many stroke survivors make significant strides in their recovery journey. With advances in medical treatment, rehabilitation techniques, and ongoing support, individuals can achieve meaningful improvements in function, independence, and quality of life. It’s essential to approach recovery with patience, perseverance, and optimism, recognizing that progress may occur gradually over time. By focusing on what is achievable and maintaining a positive mindset, stroke survivors can navigate the challenges of life after stroke with resilience and hope.
Support and Resources for Stroke Survivors:
There’s a good amount of support available for stroke survivors, both in terms of social connections and practical resources. Here’s a breakdown of what stroke survivors can access.
Social Support:
Stroke support groups: Connecting with other survivors who understand the challenges you face can be invaluable. Support groups offer a safe space to share experiences, ask questions, and provide encouragement for one another. There might be online and in-person options available in your area. You can search for groups through organizations like the American Stroke Association [American Stroke Association stroke ON stroke.org].
Informal support: Leaning on friends, family, and religious communities can provide emotional support and practical help with daily tasks.
Formal Support:
Rehabilitation services: Speech therapy, occupational therapy, and physical therapy are crucial for regaining lost abilities and improving daily functioning after a stroke. These services can be provided in hospitals, outpatient clinics, or even at home.
Aging and disability services: Government agencies offer resources and referrals for various needs, such as transportation assistance, home modifications, or personal care services.
Stroke Family Warmline: The American Stroke Association offers a helpline (1-888-4-STROKE) for stroke survivors and their families. They can provide support, information, or just a listening ear.
Additional Resources:
American Stroke Association: [American Stroke Association stroke ON stroke.org] This comprehensive website provides information on stroke prevention, treatment, recovery, and support resources.
National Institute of Neurological Disorders and Stroke: [National Institute of Neurological Disorders and Stroke (.gov)] This website from the National Institutes of Health offers detailed information on stroke research, clinical trials, and patient education resources.
Stroke Association (UK): [Stroke Association stroke ON stroke.org.uk] While this organization is based in the UK, they have a wealth of information on stroke that can be helpful for anyone.
FAQs about Brain Stroke:
A1: Risk factors for brain stroke include high blood pressure, smoking, diabetes, high cholesterol, obesity, and a sedentary lifestyle.
A2: You can reduce your risk of brain stroke by maintaining a healthy lifestyle, controlling high blood pressure, managing diabetes, quitting smoking, and staying physically active.
A3: If you suspect someone is having a stroke, remember the acronym FAST: Face drooping, Arm weakness, Speech difficulty, Time to call emergency services(Hospital). Call 911 immediately.
A4: Recovery from a brain stroke varies depending on factors such as the severity of the stroke and promptness of treatment. While some individuals may fully recover, others may have lasting effects.
A5: Stroke survivors can access support through rehabilitation programs, support groups, and resources provided by organizations like the National Stroke Association and American Stroke Association.
-Please remember, to always consult with healthcare professionals or Doctors for personalized advice related to medical conditions.
Conclusion:
Brain stroke is a serious medical condition that requires prompt recognition and treatment to minimize damage and improve outcomes. By understanding the causes, symptoms, and treatment options for stroke, individuals can take steps to reduce their risk and improve their chances of recovery.





yes what you do for me.