
HEALTH BLOG
Chronic Kidney Disease: Symptoms, Treatment and Stages
-
Rahul Priydarss
Discover comprehensive insights into Chronic Kidney Disease (CKD), covering its symptoms, treatment options, and stages. Explore Ayurvedic approaches, recent breakthroughs in pig kidney transplantation, and essential lifestyle changes. Learn how early diagnosis and intervention are crucial for managing CKD effectively and improving patient outcomes.
What is Chronic Kidney Disease (CKD):
Chronic Kidney Disease (CKD) is a condition characterized by the gradual loss of kidney function over time. The kidneys are essential organs responsible for filtering waste products and excess fluids from the blood, producing urine, regulating electrolyte levels, and maintaining overall bodily homeostasis.
Healthy kidneys also help regulate blood pressure, produce red blood cells, and keep bones strong. When CKD progresses, the kidneys lose their ability to perform these essential functions. This can lead to a buildup of waste products and fluids in the body, which can cause a variety of health problems.

Table of Contents
Causes and Risk Factors of Chronic Kidney Disease:
Understanding these causes and risk factors can help individuals take preventive measures and seek timely medical intervention to protect their kidney health. Chronic kidney disease (CKD) can develop due to various factors, including.
Diabetes: Diabetes is a leading cause of CKD. High blood sugar levels over time can damage the kidneys’ delicate filtering units.
High Blood Pressure: High blood pressure, or hypertension, can strain the kidneys, leading to CKD over time. It’s crucial to manage blood pressure to protect kidney health.
Family History: A family history of kidney disease can increase an individual’s risk of developing CKD. Genetics may play a role in predisposing someone to kidney problems.
Age: As individuals age, the risk of developing CKD increases. Aging kidneys may not function as efficiently, making them more susceptible to damage.
Smoking: Smoking can harm blood vessels and decrease blood flow to the kidneys. This can impair kidney function and contribute to the development of CKD.
Obesity: Obesity is linked to an increased risk of CKD. Excess weight can strain the kidneys and contribute to conditions like diabetes and high blood pressure.
Heart Disease: Heart disease and CKD often coexist. Conditions like coronary artery disease can affect blood flow to the kidneys, leading to kidney damage.
Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, and Native Americans, have a higher risk of developing CKD compared to others.
Prolonged Use of Certain Medications: Some medications, especially when used long-term, can cause kidney damage. It’s essential to use medications cautiously and under medical supervision.
Kidney Stones: Repeated episodes of kidney stones can impair kidney function and increase the risk of developing CKD over time.
Symptoms of Chronic Kidney Disease:
It’s important to note that not everyone with CKD will experience all of these symptoms, and symptoms may vary depending on the stage and severity of the disease. Chronic kidney disease (CKD) often progresses silently, with symptoms becoming apparent only in later stages. Some common signs and symptoms include.
Fatigue and Weakness: Feeling persistently tired or weak, even after getting enough rest, can be indicative of reduced kidney function. Anemia, a common complication of CKD, can contribute to feelings of fatigue.
Swelling in Ankles, Feet, or Hands: Retention of fluid due to impaired kidney function can lead to swelling, particularly in the lower extremities such as the ankles, feet, or hands. This swelling, known as edema, is often more noticeable later in the day.
Shortness of Breath: Buildup of waste products and fluid retention can lead to shortness of breath or difficulty breathing. This symptom may worsen with physical exertion or when lying down.
Foamy Urine: Excessive protein in the urine, known as proteinuria, can cause the urine to appear foamy or frothy. Proteinuria is a common early sign of kidney damage.
Decreased Appetite: Loss of appetite or a general feeling of malaise may occur as waste products accumulate in the body. Nausea and vomiting may also accompany decreased appetite.
Changes in Urination: Changes in urination patterns, such as increased frequency, difficulty urinating, or the need to urinate at night (nocturia), may occur in CKD. Urine may also be darker or lighter in color than usual.
Persistent Itching: Uremic pruritus, or persistent itching, is a common symptom of advanced CKD. Itching may be localized or affect the entire body and can be quite bothersome.
Muscle Cramps: Muscle cramps, particularly in the legs, may occur in individuals with CKD. These cramps can be painful and may worsen with physical activity.
Difficulty Concentrating: Reduced kidney function can lead to a buildup of toxins in the blood, affecting cognitive function. Difficulty concentrating, memory problems, and mental fog may occur.
Dry, Itchy Skin: CKD can cause dry, itchy skin due to mineral imbalances and changes in hormone levels. Skin may feel rough, scaly, or irritated.
High Blood Pressure: CKD can lead to or worsen high blood pressure, which often has no noticeable symptoms but can increase the risk of heart disease and stroke.
Changes in Heart Rhythm: Electrolyte imbalances associated with CKD can affect the heart’s rhythm, leading to palpitations or irregular heartbeats.
Swollen or Puffy Eyes: Fluid retention can cause puffiness or swelling around the eyes, particularly in the morning upon waking.
Persistent Headaches: Headaches, particularly those that are persistent or severe, may occur in individuals with CKD, often due to high blood pressure or electrolyte imbalances.
Diagnosis and Tests for Chronic Kidney Disease:
Diagnosing chronic kidney disease (CKD) typically involves a combination of medical history assessment, physical examination, and laboratory tests. Early detection is crucial for effective management and slowing the progression of the disease. Here are some common diagnostic procedures and tests used for diagnosing CKD.
Blood Tests:
Blood tests are essential for evaluating kidney function and detecting abnormalities in blood chemistry. The following blood tests are commonly used:
Serum Creatinine: Elevated levels of creatinine in the blood indicate reduced kidney function, as creatinine is a waste product that the kidneys normally filter out.
Blood Urea Nitrogen (BUN): BUN levels can indicate how well the kidneys are filtering waste from the blood. Elevated BUN levels may suggest impaired kidney function.
Glomerular Filtration Rate (GFR): GFR is a calculated value based on creatinine levels, age, gender, and other factors. It provides an estimate of the kidneys’ filtering capacity.
Electrolyte Levels: Imbalances in electrolytes such as potassium, sodium, and calcium can occur in CKD and may require monitoring and management.
Cystatin C test: This is a newer test that may be more accurate than creatinine for estimating GFR, especially in people with muscle wasting conditions.
Urine tests:
Urinalysis: This test checks for abnormalities in your urine, such as the presence of protein or blood. Protein in the urine (proteinuria) is an early sign of CKD.
Urine albumin-to-creatinine ratio (UACR): This test measures the amount of albumin, a type of protein, in your urine relative to the amount of creatinine. An elevated UACR is a sign of kidney damage.
Imaging tests:
Ultrasound: An ultrasound scan uses sound waves to create images of your kidneys. This test can help identify blockages, such as kidney stones, or abnormalities in the size or shape of your kidneys.
CT scan: A CT scan uses X-rays to create detailed cross-sectional images of your kidneys. It can provide more information about the structure of your kidneys than an ultrasound.
MRI scan: An MRI scan uses magnetic fields and radio waves to create detailed images of your kidneys. It can be especially useful for looking at blood flow to the kidneys.
Kidney biopsy:
In some cases, a kidney biopsy may be necessary to confirm a diagnosis or determine the underlying cause of kidney disease. During a kidney biopsy, a small sample of kidney tissue is removed and examined under a microscope for signs of damage or disease.
Other Tests:
Additional tests may be ordered based on individual patient characteristics and clinical presentation. These may include tests to assess blood pressure, assess cardiovascular risk, or evaluate for underlying conditions such as diabetes or autoimmune diseases.
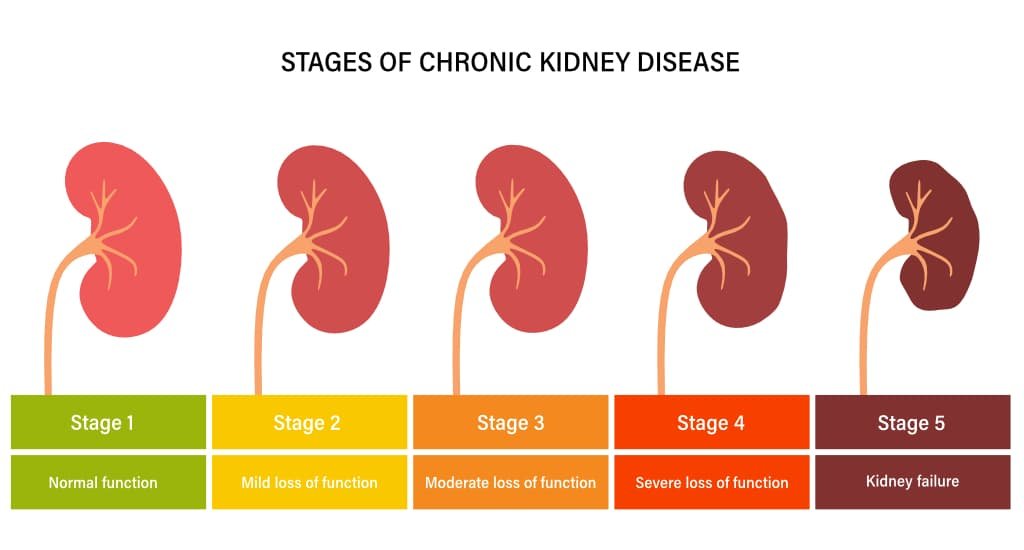
Stages of Chronic Kidney Disease:
Chronic kidney disease (CKD) is categorized into five stages based on the glomerular filtration rate (GFR), which measures kidney function. The stages range from mild kidney damage with normal GFR to kidney failure requiring dialysis or transplantation. Understanding the stages of CKD is crucial for healthcare providers to assess the severity of the disease, monitor progression, and develop appropriate treatment plans for patients. Here’s an overview of each stage.
Stage 1: Kidney Damage with Normal GFR: In Stage 1 CKD, there is evidence of kidney damage, such as proteinuria (presence of protein in the urine) or abnormal imaging studies, but the GFR is normal (>90 mL/min/1.73 m²). Kidney function is still considered normal, but there may be signs of early kidney disease.
Stage 2: Mild Decrease in GFR: In Stage 2 CKD, there is mild kidney damage, and the GFR is moderately decreased (60-89 mL/min/1.73 m²). Kidney function is slightly reduced, but individuals may not experience significant symptoms at this stage.
Stage 3: Moderate Decrease in GFR: Stage 3 CKD is further divided into two sub-stages:
- Stage 3a: GFR is moderately decreased (45-59 mL/min/1.73 m²).
- Stage 3b: GFR is moderately to severely decreased (30-44 mL/min/1.73 m²).
At this stage, kidney function is significantly impaired, and individuals may begin to experience symptoms such as fatigue, swelling, and changes in urination patterns.
Stage 4: Severe Decrease in GFR: In Stage 4 CKD, there is severe kidney damage, and the GFR is severely decreased (15-29 mL/min/1.73 m²). Kidney function is markedly impaired, and individuals may experience symptoms such as fatigue, fluid retention, and electrolyte imbalances.
Stage 5: Kidney Failure: Stage 5 CKD, also known as end-stage renal disease (ESRD), occurs when the kidneys have lost nearly all of their function, and the GFR is less than 15 mL/min/1.73 m². At this stage, the kidneys can no longer maintain adequate filtration and waste removal, leading to a buildup of toxins and fluid in the body.
“Treatment options for Stage 5 CKD include dialysis or kidney transplantation. Without intervention, Stage 5 CKD can be life-threatening.”
Treatment Options for Chronic Kidney Disease:
Treatment for chronic kidney disease (CKD) focuses on managing symptoms, slowing the progression of the disease, and preventing complications. The treatment plan may vary depending on the stage of CKD and individual patient factors. Here are some common treatment options.
Medications:
Blood Pressure Medications: Controlling high blood pressure is crucial in managing CKD. Medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are often prescribed to lower blood pressure and protect the kidneys from further damage.
Medications to Manage Complications: Depending on the specific complications present, medications may be prescribed to manage symptoms such as anemia, bone disease, or electrolyte imbalances.
Lifestyle Changes:
Healthy Diet: Following a kidney-friendly diet low in sodium, phosphorus, and potassium can help manage CKD and reduce the workload on the kidneys. A dietitian can provide personalized dietary recommendations based on individual needs.
Regular Exercise: Regular physical activity can help control blood pressure, manage weight, and improve overall health. However, exercise should be tailored to individual capabilities and medical conditions.
Smoking Cessation: Quitting smoking is essential for protecting kidney health and reducing the risk of cardiovascular complications associated with CKD.
Dialysis:
Hemodialysis: In hemodialysis, blood is filtered outside the body through a dialysis machine and returned to the body after waste products and excess fluid are removed. Hemodialysis is typically performed several times per week at a dialysis center.
Peritoneal Dialysis: Peritoneal dialysis involves using the lining of the abdomen (peritoneum) as a filter to remove waste and excess fluid from the body. It can be performed at home, allowing for more flexibility in treatment schedules.
Kidney Transplantation:
Kidney Transplant: Kidney transplantation is considered the best treatment option for eligible patients with end-stage renal disease (ESRD). A healthy kidney from a donor is surgically implanted into the recipient’s body, restoring kidney function and improving quality of life.
Complications Management:
Anemia Management: Medications such as erythropoietin-stimulating agents (ESAs) may be prescribed to stimulate red blood cell production and manage anemia associated with CKD.
Bone Disease Management: Medications and supplements may be prescribed to prevent or treat bone disease (renal osteodystrophy) associated with CKD, including calcium supplements, vitamin D analogs, and phosphate binders.
Monitoring and Follow-up:
Regular monitoring of kidney function, blood pressure, and overall health is essential for managing CKD effectively. Healthcare providers will adjust treatment plans as needed based on changes in the patient’s condition.
Ayurvedic Treatment Options for Chronic Kidney Disease:
Ayurveda, an ancient Indian system of medicine, offers holistic treatment options for chronic kidney disease (CKD) aimed at restoring balance to the body and improving kidney function. While Ayurvedic treatments should be used in conjunction with conventional medical care, they can complement traditional therapies and promote overall well-being. Here are some Ayurvedic treatment options for CKD.
Herbal Remedies:
Punarnava (Boerhavia diffusa): Punarnava is a potent diuretic herb that helps improve kidney function by promoting urine output and reducing fluid retention. It also has anti-inflammatory properties, which can benefit individuals with CKD.
Gokshura (Tribulus terrestris): Gokshura is known for its diuretic and nephroprotective properties. It helps improve kidney function, reduce inflammation, and promote the elimination of toxins from the body.
Varuna (Crataeva nurvala): Varuna is traditionally used in Ayurveda to support kidney health and treat urinary disorders. It has diuretic and anti-inflammatory properties, making it beneficial for individuals with CKD.
Dietary Recommendations:
Low Protein Diet: Ayurvedic principles recommend reducing the intake of protein-rich foods to lessen the burden on the kidneys. Instead, emphasis is placed on consuming easily digestible, plant-based proteins and avoiding excessive consumption of animal proteins.
Herbal Teas and Decoctions: Drinking herbal teas or decoctions made from kidney-supportive herbs such as Punarnava, Gokshura, and Varuna can help promote kidney health and support detoxification.
Hydration: Adequate hydration is essential for kidney function. Drinking plenty of fluids, especially warm water, can help flush out toxins and support overall kidney health.
Lifestyle Modifications:
Yoga and Meditation: Practicing yoga asanas (poses) and meditation techniques can help reduce stress, promote relaxation, and improve overall well-being. Stress reduction is important for individuals with CKD, as stress can exacerbate symptoms and contribute to disease progression.
Regular Exercise: Engaging in gentle, low-impact exercises such as walking, swimming, or yoga can improve circulation, strengthen the body, and support kidney function. However, individuals with CKD should consult with a healthcare provider before starting any exercise program.
Panchakarma Therapy:
Panchakarma: Panchakarma is a detoxification and rejuvenation therapy in Ayurveda that involves various cleansing procedures to remove toxins from the body and restore balance to the doshas (bioenergies). Panchakarma therapies such as Virechana (purgation) and Basti (enema) can be beneficial for individuals with CKD to support detoxification and promote kidney health.
Ayurvedic Consultation:
It’s essential for individuals with CKD to consult with a qualified Ayurvedic practitioner for personalized treatment recommendations based on their unique constitution and health condition. Ayurvedic treatments should be tailored to individual needs and used under the guidance of a trained professional to ensure safety and efficacy.
New Achievement on Pig Kidney Transplant in 2024:
In a landmark achievement in the field of medicine, a 62-year-old man has been discharged from Massachusetts General Hospital (MGH) following a groundbreaking kidney transplant procedure. According to a report by BBC, this historic event marks the first successful kidney transplant from a genetically modified pig, signifying a significant breakthrough in organ transplantation.
The Breakthrough:
First Successful Pig Kidney Transplant: Doctors at Massachusetts General Hospital performed the world’s first successful transplant of a genetically modified pig kidney into a living human recipient in March 2024 [https://www.massgeneral.org/news/press-release/worlds-first-genetically-edited-pig-kidney-transplant-into-living-recipient].
Recipient Recovery: The recipient, 62-year-old Richard Slayman, recovered well and was discharged from the hospital just two weeks after surgery [https://khagapharmacy.com/pig-kidney-transplant-the-way/].
Genetically Modified Pig: The transplanted kidney came from a pig genetically engineered using CRISPR-Cas9 technology. This removed harmful pig genes and added specific human genes to make the organ more compatible with the human body and reduce rejection [https://www.bmj.com/content/384/bmj.q731].
FAQs about Chronic Kidney Disease:
A1: While family history can increase the risk of CKD, it’s not solely determined by genetics. Lifestyle factors also play a significant role.
A2: In most cases, CKD cannot be cured, but early detection and treatment can help slow its progression and manage complications effectively.
A3: Dialysis is one option for managing kidney failure, but kidney transplantation offers a more long-term solution for eligible patients.
A4: While some risk factors for CKD are beyond control, such as age and family history, adopting a healthy lifestyle can help reduce the risk and delay the onset of the disease.
A5: The frequency of medical monitoring for individuals with CKD depends on the stage of the disease and their overall health. It’s important to follow the recommendations of healthcare professionals for regular check-ups and tests.

-Please remember, to always consult with healthcare professionals or Doctors for personalised advice related to medical conditions.
Conclusion:
In summary, Chronic Kidney Disease (CKD) poses a significant health risk, with gradual kidney function loss over time. Understanding its causes, symptoms, and stages is crucial for timely diagnosis and management. Ayurvedic therapies offer holistic support, while recent breakthroughs in pig kidney transplantation show promise for future treatments. Regular medical monitoring and lifestyle changes are vital for slowing CKD progression and improving outcomes. Early intervention is key to managing CKD effectively and enhancing patient well-being.




