
HEALTH NEWS
Bubonic Plague: From Black Death to 2024 Modern Concerns
-
Rahul Priydarss
Explore the journey of the bubonic plague from its historic havoc to its modern-day concerns in 2024. Understand its origins, transmission, and historical impact, including the infamous Black Death. Learn about recent cases and the potential for animal-to-human transmission, stressing the need for awareness and preparedness today. Discover the differences between past and present outbreaks, highlighting advancements in medicine and public health. Get insights into global prevalence, affected regions, symptoms, diagnosis, and treatment, along with a scenario of a 2024 outbreak. Understand risk factors, public awareness, and future outlook. Stay informed and ready to tackle this enduring public health challenge.
What is Bubonic Plague:
The bubonic plague, one of the most infamous diseases in human history, has left an indelible mark on civilization through its devastating impact on populations over the centuries. Understanding its origins, transmission, and historical context is essential in comprehending its significance in both the past and present.
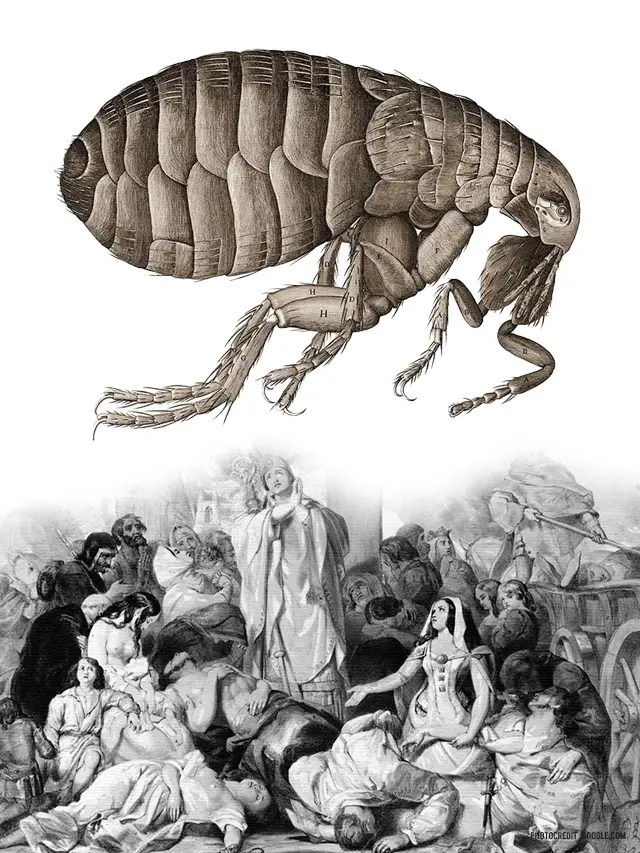
Bubonic Plague is a severe infectious disease caused by the bacterium Yersinia pestis. It is primarily transmitted through the bite of infected fleas that typically reside on rodents like rats. While bubonic plague is rare in modern times, it has a notorious history as one of the deadliest diseases humanity has faced. The most infamous pandemic, known as the Black Death, occurred in the 14th century and wiped out millions of lives in Europe.
The bubonic plague, a disease that ravaged Europe in the Middle Ages, continues to exist in the 21st century. While not a widespread threat, recent cases in 2024 serve as a reminder of the importance of awareness and preparedness.

Table of Contents
History of Bubonic Plague:
The bubonic plague, caused by the bacterium Yersinia pestis, first made its mark on human history during the Justinian Plague in the 6th century. However, its most notorious episode occurred during the 14th century with the outbreak known as the Black Death. This pandemic, originating in Asia, swept through Europe, claiming millions of lives and reshaping the social, economic, and cultural landscape of the continent.
A Cause for Concern:
In February 2024, a case of bubonic plague was confirmed in rural Oregon, raising concerns. The individual likely contracted the disease from their pet cat, highlighting the potential for transmission from animals to humans. Thankfully, health officials were able to identify and treat the case early, preventing further spread within the community.
This incident underscores the fact that the bubonic plague, though uncommon, remains a zoonotic disease – meaning it can jump from animals to humans. Rodents, particularly squirrels, prairie dogs, and chipmunks serve as natural reservoirs for the plague bacteria, Yersinia pestis. Fleas that feed on these infected rodents can then transmit the bacteria to humans through bites.
Past Outbreaks of Bubonic Plague: A Shadowy History:
The bubonic plague, a horrifying disease marked by swollen lymph nodes and high mortality rates, has cast a long shadow on human history. Here’s a look at its two most infamous periods:
The Black Death: A Devastating Scourge (1347-1351): The Black Death, the most notorious bubonic plague pandemic, ravaged Europe in the mid-14th century. It’s estimated to have wiped out 30-50% of Europe’s population within a few short years. The origins of the Black Death remain debated, but it’s believed to have originated in Central Asia before spreading westward along trade routes. Infected fleas on rodents likely played a major role in transmission.
Cities with poor sanitation and cramped living conditions proved breeding grounds for the disease. Symptoms like fever, chills, and buboes were terrifying and often fatal. The lack of effective treatments at the time meant the plague spread like wildfire.
The Black Death’s social and economic impact was profound. It disrupted labor markets, led to widespread fear and social unrest, and significantly altered the course of European history.
Modern Outbreaks: A Persistent Threat: While the Black Death remains the most devastating bubonic plague outbreak, the disease hasn’t vanished. Outbreaks continue to occur, particularly in parts of Africa, Asia, and South America. The good news is that modern medicine has changed the game. Antibiotics like tetracycline and streptomycin are highly effective against the plague bacteria if caught early. Additionally, public health measures like flea control and improved sanitation significantly reduce the risk of large-scale outbreaks.
Here are some examples of modern bubonic plague outbreaks:
- Third Pandemic (1894-1920s): This pandemic originated in China and spread to port cities worldwide through infected rats on ships. Outbreaks occurred in Hong Kong, India, and San Francisco.
- Madagascar: The country experiences periodic outbreaks, with the most recent significant one in 2017.
Key Differences Between Past and Present:
The bubonic plague of today differs significantly from the Black Death.
- Treatment: Modern antibiotics make the disease highly treatable if diagnosed promptly.
- Public Health Measures: Improved sanitation and flea control significantly reduce the risk of outbreaks.
- Global Awareness: Early detection and response mechanisms are in place to prevent widespread pandemics.
The Bubonic Plague: A Global Snapshot in 2024:
The bubonic plague may seem like a relic of the past, but it remains a zoonotic disease, meaning it can jump from animals to humans. While not a widespread threat in 2024, understanding its current prevalence and affected regions is crucial.
Global Prevalence: A Low But Persistent Threat: The World Health Organization (WHO) estimates an average of around 1,700 cases of bubonic plague reported globally each year. This may seem like a significant number, but it’s important to consider.
- This is a global average, and the vast majority of cases are concentrated in specific regions.
- Modern antibiotics are highly effective against the plague bacteria if diagnosed early.
Affected Regions: A Geographical Hotspot: The bubonic plague isn’t evenly distributed around the world. Here’s a breakdown of the most affected regions in 2024.
- Africa: The Democratic Republic of Congo consistently reports the highest number of cases globally.
- Asia: Countries like China, Mongolia, and Kazakhstan also experience occasional outbreaks.
- South America: Peru and Bolivia have documented cases of bubonic plague in recent years.
A Look at the United States: The United States sees a relatively low number of cases compared to the regions mentioned above. The Centers for Disease Control and Prevention (CDC) reports an average of seven human plague cases per year, primarily concentrated in the western states.
- Areas with high concentrations of wild rodents, particularly squirrels and prairie dogs, serve as natural reservoirs for the plague bacteria.
- States like New Mexico, Arizona, Colorado, California, Oregon, and Nevada have reported cases in recent years.
It’s important to note:
- The 2024 case in Oregon highlights the possibility of sporadic cases even outside typical hotspots.
- Public health measures and awareness campaigns play a vital role in preventing outbreaks in the US.
Symptoms of Bubonic Plague:
Bubonic plague manifests with a distinct set of symptoms, typically appearing within a few days to a week after exposure to the bacterium Yersinia pestis. Recognizing these symptoms is essential for prompt diagnosis and treatment to prevent complications and further transmission of the disease.
Fever: One of the hallmark symptoms of bubonic plague is the sudden onset of fever, often accompanied by chills and rigors. The fever may spike rapidly, reaching high temperatures.
- Early Flu-like Symptoms (1-7 days after exposure):
- Sudden high fever (often exceeding 102°F or 38.9°C)
- Chills
- Headache
- Weakness
- Nausea and vomiting
Swollen Lymph Nodes (Buboes): Bubonic plague derives its name from the characteristic swollen lymph nodes, known as buboes, that develop in affected individuals.
- One to seven days after the initial flu-like symptoms, the most characteristic sign of bubonic plague develops swollen and painful lymph nodes (buboes). These typically appear in the:
- Groin
- Armpit
- Neck
Pain and Tenderness: Individuals with bubonic plague may experience localized pain and tenderness around the site of the swollen lymph nodes. The affected area may feel warm to the touch and appear red or inflamed.
- Headache: Many patients with bubonic plague report experiencing severe headaches, which may be persistent and debilitating. Headaches often accompany the fever and contribute to feelings of malaise and discomfort.
- Fatigue and Weakness: Bubonic plague can cause profound fatigue and weakness, making it difficult for affected individuals to perform daily activities. The combination of fever, pain, and other symptoms can lead to significant fatigue and lethargy.
- Nausea and Vomiting: Some individuals with bubonic plague may experience gastrointestinal symptoms such as nausea and vomiting. These symptoms can contribute to dehydration and further exacerbate feelings of weakness and malaise.
- Muscle Aches and Joint Pain: Muscle aches and joint pain are common manifestations of bubonic plague, often contributing to the overall discomfort experienced by affected individuals. These symptoms may worsen with movement or pressure on the affected areas.
Other Symptoms: In severe cases or if left untreated, bubonic plague can progress to more severe forms, such as septicemic or pneumonic plague, which present with additional symptoms such as cough, difficulty breathing, chest pain, and disorientation.
- Severe fatigue and malaise
- Muscle aches
- Shortness of breath
- Skin discoloration or necrosis (tissue death) near the buboes in severe cases
Diagnosis of Bubonic Plague:
Diagnosing bubonic plague involves a combination of clinical evaluation, laboratory testing, and epidemiological investigation to confirm the presence of the disease and guide appropriate treatment and public health interventions.
Clinical Presentation:
Initial Evaluation: piecing together the puzzle
Doctors will first gather information about your medical history, including.
- Symptoms: A detailed description of your symptoms, including their onset and severity, is crucial.
- Travel history: Recent travel to areas with known plague activity can raise suspicion.
- Potential exposure: Contact with wild rodents, fleas, or sick individuals can be a significant clue.
Bubonic plague typically presents with nonspecific symptoms that can initially resemble other common illnesses, making diagnosis challenging. The hallmark symptoms include the sudden onset of fever, chills, headache, muscle aches, and fatigue. However, the most distinctive feature of bubonic plague is the development of painful, swollen lymph nodes, known as buboes, which are often located in the groin, armpit, or neck. These swollen lymph nodes can rapidly become tender and inflamed, leading to the characteristic bubonic form of the disease.
Diagnostic Methods:
- Clinical Assessment: Healthcare providers evaluate patients presenting with symptoms suggestive of bubonic plague, including a thorough medical history, physical examination, and assessment of risk factors such as recent travel to endemic regions or exposure to rodents and fleas.
- Laboratory Tests: Laboratory testing plays a crucial role in confirming the diagnosis of bubonic plague. Samples collected from patients, such as blood, sputum, or tissue aspirates from buboes, are examined for the presence of the bacterium Yersinia pestis. Techniques such as polymerase chain reaction (PCR), culture, and antigen detection tests help identify the specific pathogen responsible for the infection. Several laboratory tests can be used to confirm or rule out bubonic plague.
- Blood tests: These can detect the presence of the plague bacteria (Yersinia pestis) or antibodies your body produces in response to the infection.
- Aspiration of pus from a bubo: If a swollen lymph node is present, a needle can be used to extract a sample of pus for testing. This can directly identify the plague bacteria.
- Sputum test (for pneumonic plague): If pneumonic plague is suspected, a sample of mucus coughed up from the lungs will be analyzed for the presence of Yersinia pestis.
Rapid Diagnostic Tests:
- In some cases, rapid diagnostic tests may be used to expedite diagnosis. These tests, while not definitive, can provide a quick indication of potential plague infection:
- F1 antigen tests: These tests detect a specific antigen produced by the plague bacteria. They can be performed using dipsticks or other methods and offer relatively quick results.
- Imaging Studies: In severe cases or when complications arise, imaging studies such as X-rays or ultrasound may be performed to evaluate the extent of lymph node involvement or detect signs of pneumonia, septicemia, or other systemic complications associated with advanced stages of the disease.
Differential Diagnosis:
Given the nonspecific nature of early symptoms, healthcare providers must consider a wide range of differential diagnoses when evaluating patients suspected of having bubonic plague. Differential diagnoses may include other infectious diseases such as influenza, septicemia, or other causes of lymphadenopathy such as lymphoma or infectious mononucleosis. A thorough evaluation, including laboratory testing and clinical correlation, is essential to differentiate bubonic plague from other potential causes of illness.

Treatment of Bubonic Plague:
Effective treatment of bubonic plague is essential for reducing mortality rates and preventing the spread of the disease. Prompt diagnosis and initiation of appropriate therapy are crucial in managing cases of bubonic plague and minimizing its impact on affected individuals and communities.
Antibiotic Therapy: The cornerstone of treatment for bubonic plague is antibiotic therapy. Several antibiotics have proven efficacy against Yersinia pestis, the bacterium responsible for causing the disease. Among the most commonly used antibiotics are.
- Streptomycin: This antibiotic is highly effective against Yersinia pestis and is often the first-line treatment for bubonic plague. It works by inhibiting bacterial protein synthesis, ultimately leading to bacterial cell death.
- Gentamicin: Another antibiotic belonging to the aminoglycoside class, gentamicin, demonstrates potent activity against Yersinia pestis. It functions similarly to streptomycin by interfering with bacterial protein synthesis.
- Doxycycline: A broad-spectrum antibiotic belonging to the tetracycline class, doxycycline, is often used as an alternative treatment for bubonic plague. It inhibits bacterial protein synthesis and is effective against a wide range of pathogens, including Yersinia pestis.
- Ciprofloxacin: A fluoroquinolone antibiotic, ciprofloxacin, is sometimes used as an alternative therapy for bubonic plague. It works by inhibiting bacterial DNA gyrase and topoisomerase IV, essential enzymes involved in bacterial DNA replication and repair.
Supportive Care: In addition to antibiotic therapy, supportive care plays a crucial role in managing bubonic plague cases. Supportive measures may include:
- Fluid and electrolyte management: Intravenous fluids may be administered to maintain hydration and electrolyte balance, particularly in cases of severe dehydration or electrolyte disturbances.
- Pain management: Analgesic medications may be prescribed to alleviate pain and discomfort associated with swollen lymph nodes (buboes) or other symptoms of bubonic plague.
- Monitoring and surveillance: Close monitoring of vital signs, laboratory parameters, and clinical status is essential to assess the patient’s response to treatment and detect any complications early.
Isolation and Infection Control: Patients diagnosed with bubonic plague should be isolated to prevent the spread of the disease to others. Infection control measures, including wearing personal protective equipment (PPE), practicing proper hand hygiene, and implementing environmental disinfection protocols, are essential to minimize the risk of transmission in healthcare settings.
Preventive Measures: Preventive measures play a crucial role in controlling the spread of bubonic plague within communities. These measures may include.
- Vector control: Implementing strategies to control fleas and rodent populations, such as using insecticides and rodenticides, can help reduce the risk of transmission.
- Public health education: Educating communities about the signs and symptoms of bubonic plague, as well as preventive measures such as avoiding contact with rodents and fleas, is essential in raising awareness and promoting early detection and treatment.
- Vaccination: While no commercially available vaccine specifically targets bubonic plague, research into vaccine development continues, with some promising candidates showing efficacy in animal studies. Vaccination may play a role in future prevention efforts once a safe and effective vaccine becomes available.
2024 Scenario of bubonic plague:
Here’s a possible scenario of a bubonic plague outbreak in 2024, with a twist.
The Unexpected Origin:
- Unlike the typical scenario involving wild rodents, this outbreak started at a music festival held on a large outdoor property in California.
- Unbeknownst to the organizers, the festival grounds are home to a colony of feral cats.
- These cats, though not the usual culprits, can also carry and transmit the plague bacteria through fleas.
The Chain Reaction Begins:
- A festival attendee gets bitten by an infected flea while camping on the festival grounds.
- They return home to a major city on the East Coast, unknowingly carrying the plague bacteria.
- A few days later, they experience flu-like symptoms and develop a swollen lymph node (bubo) in their groin.
A Different Path to Diagnosis:
- Due to the rarity of bubonic plague and the lack of connection to a known plague zone, the initial diagnosis might be misconstrued as a more common infection.
- However, the patient’s recent travel history to the music festival raises a red flag for a doctor familiar with potential plague risks.
Amplifying the Threat:
- By the time the bubonic plague is confirmed, the infected individual has spent several days in close quarters with friends and family back east.
- This increases the risk of potential secondary cases, especially if the infected individual wasn’t practicing proper hygiene while symptomatic.
A Race Against Time:
- Public health officials scramble to identify and contact everyone who may have been exposed at the festival and during the patient’s travels.
- This large-scale contact tracing effort proves challenging due to the transient nature of festival attendees.
Containing the Outbreak:
- Luckily, the swift response and immediate antibiotic treatment of the initial case prevent further spread within their close circle.
- However, a few secondary cases are identified among festival attendees who had contact with the infected individual and also developed symptoms.
Lessons Learned (with a Modern Twist):
- This scenario highlights the potential for bubonic plague to spread outside typical high-risk areas through unexpected vectors like feral cats.
- It emphasizes the importance of public awareness about bubonic plague symptoms, even in low-risk regions.
- Large-scale events like music festivals pose a unique challenge for contact tracing in case of an outbreak.
The Road to Recovery:
- Thanks to prompt diagnosis and treatment, all identified cases make a full recovery.
- The music festival incident serves as a wake-up call, prompting public health officials to issue warnings about bubonic plague risks and preventive measures, particularly for outdoor activities in areas with potential wild animal populations.
Risk Factors from Bubonic Plague:
Understanding the risk factors associated with bubonic plague transmission and its broader socioeconomic implications is crucial for effective prevention and control measures. Environmental factors and socioeconomic conditions play significant roles in shaping the vulnerability of populations to the disease.
Environmental Factors:
- Presence of Rodent Reservoirs: Bubonic plague is primarily a zoonotic disease, with rodents serving as the main reservoirs for the bacterium Yersinia pestis. Environments with high rodent populations, such as rural areas or densely populated urban slums, are at increased risk of disease transmission.
- Ecological Changes: Environmental disturbances, including deforestation, climate change, and habitat destruction, can disrupt ecosystems and lead to shifts in rodent populations. These changes may create new opportunities for human-animal interactions and increase the likelihood of disease spillover from rodents to humans.
- Vector Habitat: Fleas, the vectors responsible for transmitting Yersinia pestis from rodents to humans, thrive in certain environmental conditions. Factors such as temperature, humidity, and vegetation cover can influence flea abundance and distribution, affecting the risk of bubonic plague transmission in endemic regions.
- Sanitation and Hygiene Practices: Poor sanitation infrastructure, lack of access to clean water, and inadequate waste management contribute to environmental conditions conducive to the proliferation of rodents and fleas. Communities with limited resources for maintaining proper hygiene are at heightened risk of bubonic plague outbreaks.
Socioeconomic Implications:
- Poverty and Overcrowding: Socioeconomically disadvantaged communities are disproportionately affected by bubonic plague due to factors such as poverty, overcrowded living conditions, and limited access to healthcare. These populations may lack the resources to implement effective rodent control measures or seek timely medical care, increasing their vulnerability to the disease.
- Healthcare Access: Limited access to healthcare facilities and diagnostic services in rural or remote areas can delay the diagnosis and treatment of bubonic plague cases, leading to poorer health outcomes and higher mortality rates. Inadequate healthcare infrastructure further exacerbates the burden of the disease on vulnerable populations.
- Displacement and Migration: Conflict, natural disasters, and environmental degradation can force populations to migrate or seek refuge in overcrowded displacement camps or informal settlements. These settings often lack basic amenities and sanitation, increasing the risk of disease transmission, including bubonic plague, among displaced populations.
- Economic Disruptions: Bubonic plague outbreaks can have significant economic repercussions, disrupting livelihoods, trade, and agricultural activities in affected regions. Loss of productivity due to illness or death, as well as costs associated with healthcare and outbreak response, can further strain already fragile economies and exacerbate poverty.
Public Awareness and Education for the Bubonic Plague:
Public awareness and education play pivotal roles in preventing and controlling the spread of bubonic plague. By disseminating accurate information and dispelling misconceptions and myths surrounding the disease, communities can empower individuals to take proactive measures to protect themselves and their loved ones.
Importance of Knowledge Dissemination:
- Early Recognition of Symptoms: Educating the public about the signs and symptoms of bubonic plague, such as fever, chills, swollen lymph nodes (buboes), and flu-like illness, enables individuals to recognize potential cases early and seek prompt medical attention. Early diagnosis and treatment are critical for improving patient outcomes and preventing further transmission of the disease.
- Preventive Measures: Public awareness campaigns can inform communities about preventive measures to reduce the risk of bubonic plague transmission. These measures may include avoiding contact with rodents and fleas, practicing good hygiene, using insect repellents, and implementing rodent control strategies in residential and commercial settings.
- Understanding Transmission Routes: By understanding how bubonic plague is transmitted, individuals can take steps to minimize their exposure to infected rodents and fleas. Knowledge about the role of fleas as vectors and the importance of flea control measures, such as insecticide treatment and pet care, can help prevent the spread of the disease.
- Promoting Community Engagement: Public awareness initiatives encourage community members to actively participate in disease prevention and control efforts. Engaging with local health authorities, participating in vector control programs, and supporting community-based surveillance activities foster a sense of ownership and collective responsibility in addressing the threat of bubonic plague.
Misconceptions and Myths:
- Association with the Past: One common misconception is that bubonic plague is a disease of the past and no longer poses a significant threat in the modern era. However, sporadic outbreaks still occur in certain regions, highlighting the continued relevance of the disease as a public health concern.
- Fear of Contagion: Some individuals may harbor fears of contagion and avoid seeking medical care or interacting with affected individuals or communities. Educating the public about the modes of transmission and the effectiveness of modern treatments can help alleviate unfounded fears and promote compassionate and informed responses to bubonic plague cases.
- Stigmatization and Discrimination: Misconceptions about bubonic plague may lead to stigmatization and discrimination against individuals or communities perceived to be at higher risk of infection. Public awareness campaigns should emphasize the importance of empathy, solidarity, and non-discrimination in addressing the disease and supporting affected populations.
- Efficacy of Traditional Remedies: In some cultures, traditional remedies or alternative treatments are believed to cure or prevent bubonic plague. However, these practices may lack scientific evidence and could delay or undermine effective medical interventions. Encouraging individuals to seek guidance from qualified healthcare professionals ensures that they receive appropriate care based on scientific evidence and best practices.
Future Outlook for Bubonic Plague:
The Bubonic Plague: A Look Towards the Future: The bubonic plague may seem like a relic of the past, but it remains a zoonotic disease with the potential to re-emerge. Here’s a glimpse into the possible future of bubonic plague, exploring both emerging threats and advancements in research and development.
Emerging Threats:
- Antibiotic Resistance: One of the biggest concerns is the potential for antibiotic resistance. Overuse and misuse of antibiotics can lead to the emergence of plague strains resistant to commonly used antibiotics. This could significantly complicate treatment and increase mortality rates.
- Climate Change: Warming temperatures and changes in weather patterns could lead to an expansion of the geographic range of rodents and fleas that carry the plague bacteria. This could increase the risk of outbreaks in new areas.
- Bioterrorism: Though a less likely scenario, bubonic plague is classified as a potential biological weapon. The deliberate release of the bacteria could have devastating consequences.
Research and Development Efforts: Despite these looming threats, advancements are being made in research and development.
- Developing New Antibiotics: Scientists are continuously working on developing new antibiotics effective against plague bacteria, even those exhibiting some resistance.
- Improved Diagnostics: Faster and more reliable diagnostic tests for bubonic plague are being explored. This would allow for earlier intervention and prevent outbreaks.
- Vaccine Development: While no commercially available vaccine exists for bubonic plague, research is ongoing. A successful vaccine would be a significant step forward in preventing the disease.
- Surveillance and Monitoring: Enhanced global surveillance of plague activity in animals and humans can help identify potential outbreaks early and prevent their spread.
FAQs about Bubonic Plague:
A1: Yes, although rare, outbreaks of bubonic plague still occur, particularly in regions with poor sanitation.
A2: Bubonic plague is typically transmitted through the bite of infected fleas or direct contact with infected animals.
A3: Avoiding contact with rodents and fleas, practicing good hygiene, and seeking prompt medical attention if symptoms develop are crucial preventive measures.
A4: Currently, there is no commercially available vaccine for bubonic plague, but research is ongoing in this area.
A5: Seek medical attention immediately, especially if you develop symptoms such as fever, chills, and swollen lymph nodes.
-Please remember, to always consult with healthcare professionals or Doctors for personalized advice related to medical conditions.
Conclusion:
In conclusion, while the bubonic plague may seem like a relic of the past, it still poses a threat in certain parts of the world. Understanding the disease, implementing effective control measures, and fostering global cooperation are essential in preventing its resurgence.




