This comprehensive guide covers its symptoms, causes, diagnostic methods, treatment options, and prevention strategies. Written by a health expert with experience in liver health, this blog helps you understand the importance of early diagnosis and lifestyle changes. Ideal for patients, caregivers, and those at risk of liver disease.
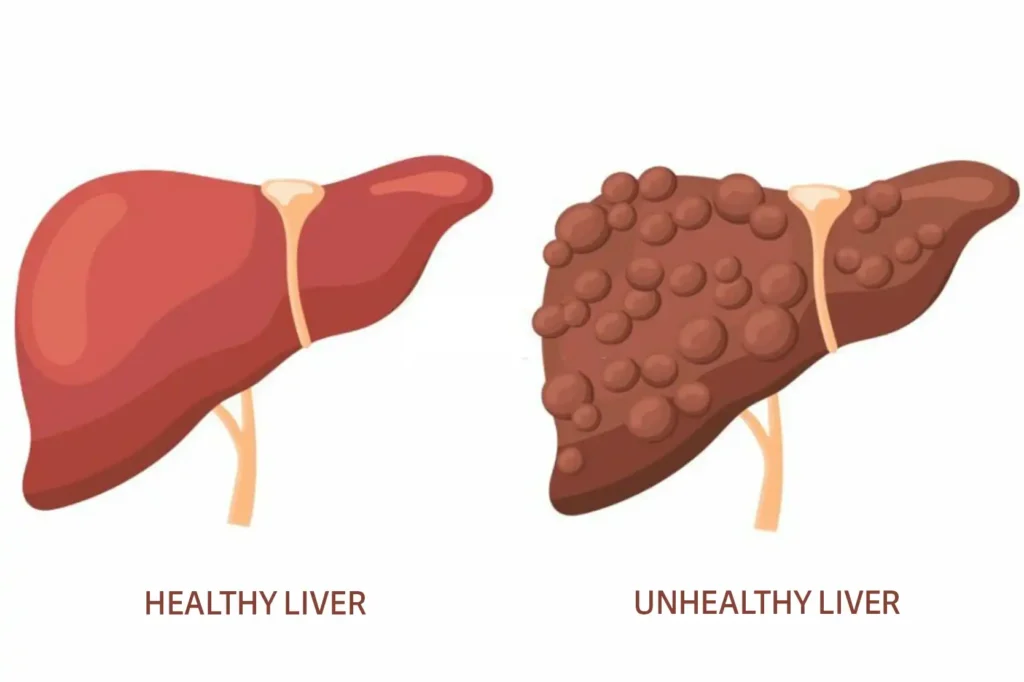
What is Diffuse Hepatocellular Disease:
Diffuse hepatocellular disease refers to a broad pattern of liver damage that impacts the liver cells (hepatocytes) uniformly, rather than being limited to one area. This damage can be caused by several factors viral infections like hepatitis B or C, chronic alcohol consumption, fatty liver disease (NAFLD/NASH), autoimmune disorders, and long-term medication use. The condition alters the liver’s ability to process toxins, store nutrients, and filter the blood putting the entire body at risk.
Unlike focal liver diseases that affect specific regions, diffuse hepatocellular disease creates a widespread pattern of injury across the liver. This condition is often diagnosed through liver function tests, ultrasound, CT scans, or liver biopsies. If left untreated, it can lead to serious complications like cirrhosis, liver failure, or hepatocellular carcinoma (liver cancer). Early detection and lifestyle management play a key role in improving outcomes.
Short-term plans are affordable but may lack comprehensive benefits like preventive care or maternity coverage.
Symptoms of Diffuse Hepatocellular Disease:
Diffuse hepatocellular disease can often remain silent in the early stages, which makes routine screening crucial, especially if you’re at risk. However, as the damage spreads, several telltale signs begin to appear. In advanced stages, confusion and memory issues may develop due to hepatic encephalopathy a result of toxins building up in the brain because the liver can no longer filter them effectively.
- Persistent fatigue
- Yellowing of the skin and eyes (jaundice)
- Nausea or vomiting
- Loss of appetite
- Abdominal swelling or pain (especially in the upper right quadrant)
- Dark urine and pale stools

Causes and Risk Factors:
There are several underlying causes of diffuse hepatocellular disease. Certain individuals are more vulnerable those with obesity, diabetes, high cholesterol, or a family history of liver disease. People who have undergone chemotherapy or long-term steroid therapy may also be at risk.
- Chronic viral hepatitis (especially Hepatitis B and C)
- Alcoholic liver disease from long-term heavy drinking
- Non-alcoholic fatty liver disease (NAFLD) and NASH (non-alcoholic steatohepatitis)
- Autoimmune hepatitis
- Drug-induced liver injury, from medications like acetaminophen or long-term antibiotics
- Exposure to toxins, like aflatoxins or industrial chemicals.
Benefits of the Marketplace:
- Subsidies and Premium Tax Credits: Many individuals and families qualify for financial assistance based on income.
- Comprehensive Coverage: Marketplace plans must cover essential health benefits, such as preventive care, emergency services, and maternity care.
- Diverse Options: Plans are available in four categories—Bronze, Silver, Gold, and Platinum—allowing you to choose based on premium costs and out-of-pocket expenses.
Diagnosis and Imaging Techniques:
Detecting diffuse hepatocellular disease often begins with routine liver function tests (LFTs). These blood tests measure enzymes like ALT, AST, and bilirubin levels. Elevated levels often suggest liver cell damage. In some cases, a liver biopsy is needed. It gives a microscopic view of liver tissue, showing the extent of inflammation, fibrosis, or fat accumulation. Biopsy remains the gold standard in assessing the severity of diffuse hepatocellular disease.
To confirm the diagnosis, imaging tests like:
- Ultrasound (to detect changes in liver texture)
- CT scan or MRI (to visualize inflammation, fat accumulation, or fibrosis)
- Transient elastography (FibroScan – to measure liver stiffness)
Treatment Options:
The treatment of diffuse hepatocellular disease largely depends on the underlying cause. In severe cases, such as advanced cirrhosis or liver failure, liver transplantation may be the only option. Regular monitoring with liver imaging and lab tests is essential to prevent progression.
- Antiviral therapy for chronic hepatitis B or C
- Lifestyle changes (diet, exercise, no alcohol) for NAFLD/NASH
- Corticosteroids or immunosuppressants for autoimmune hepatitis
- Antioxidants and liver-protective supplements like silymarin (milk thistle)
Complications of Diffuse Hepatocellular Disease:
If left untreated, diffuse hepatocellular disease can lead to serious complications. Early intervention and managing the root cause can slow or even reverse some of these complications in their early stages.
- Cirrhosis – irreversible liver scarring that affects blood flow and liver function
- Portal hypertension – increased pressure in the portal vein causing varices or ascites
- Hepatocellular carcinoma – a type of primary liver cancer
- Hepatic encephalopathy – mental confusion from toxin buildup
- Coagulopathy – poor blood clotting due to reduced liver protein production
Prevention and Lifestyle Management:
Preventing diffuse hepatocellular disease involves lifestyle choices and health monitoring. Incorporating exercise, managing cholesterol, and keeping blood sugar levels in check are also essential. Liver health is closely linked to metabolic health.
- Maintain a healthy weight to prevent NAFLD
- Avoid excessive alcohol intake
- Get vaccinated against hepatitis A and B
- Use medications cautiously and avoid unnecessary over-the-counter drugs
- Eat a balanced diet, rich in antioxidants and fiber
- Get regular checkups and liver function tests, especially if you’re at risk
FAQ
Most frequent questions and answers
In early stages, it’s often manageable or reversible especially if caused by fatty liver or hepatitis. Advanced cases may require long-term treatment.
Diffuse liver disease affects the whole liver, while focal liver disease affects one part like a localized tumor or cyst.
In cases like NAFLD, diet and weight loss can significantly reverse liver damage. But underlying infections or autoimmune issues may need medical treatment.
Conclusion:
Whether caused by viral infections, alcohol, or fatty liver, early detection and proper management are crucial to prevent long-term damage. In conclusion, diffuse hepatocellular disease is a serious liver condition that affects the entire liver, often developing silently until complications arise. By understanding its symptoms, risk factors, and treatment options, individuals can take proactive steps toward liver health. Regular checkups, a balanced lifestyle, and medical guidance can significantly slow the progression of diffuse hepatocellular disease.