
HEALTH BLOG
Mitochondrial Disease: Unveiling the Mystery Behind Cellular Dysfunction
-
 Rahul Priydarss
Rahul Priydarss - April 25, 2024
Discover the intricacies of mitochondrial disease, a group of disorders affecting cellular energy production. From understanding the role of mitochondria to exploring various types and causes of the disease, delve into its symptoms, diagnosis, and treatment options. Learn about recent research advancements, debunk common myths, and find answers to frequently asked questions. Empower yourself with knowledge about mitochondrial disease and its management in this comprehensive guide.
What is Mitochondrial Disease:
Mitochondrial disease is a group of disorders that affect the mitochondria, which are tiny compartments present in almost every cell of the body. The mitochondria’s main function is to produce energy, like the cell’s powerhouses. More mitochondria are needed to make more energy, particularly in high-energy-demand organs such as the heart, muscles, and brain. These disorders can result from nuclear or mitochondrial DNA mutations, leading to dysfunctional mitochondria.

Table of Contents
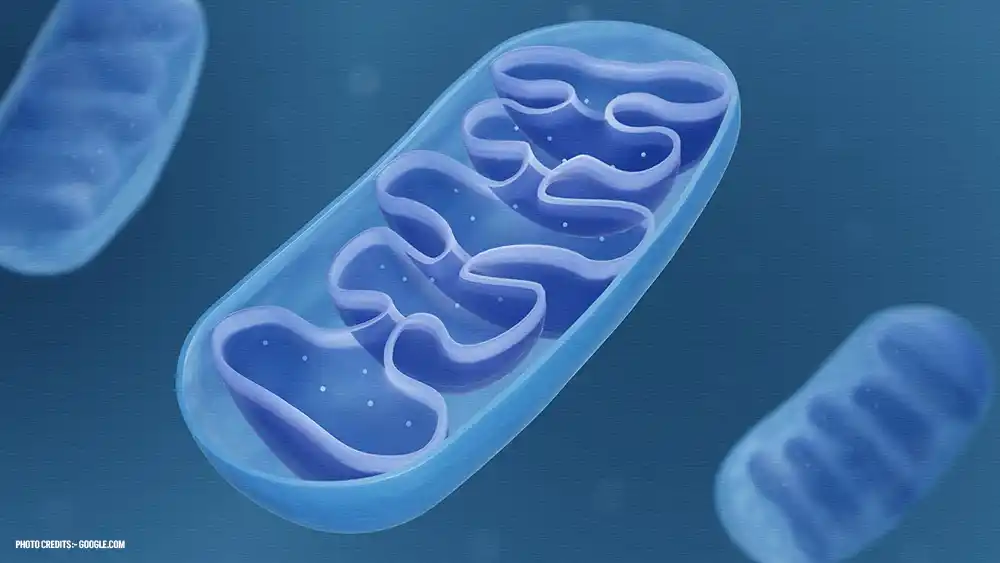
Understanding Mitochondria and Their Function:
Mitochondria are vital cellular organelles responsible for producing energy in the form of adenosine triphosphate (ATP). Found in the cytoplasm of almost all eukaryotic cells, mitochondria play a crucial role in various cellular processes.
Structure: Mitochondria have a distinctive double membrane structure. The outer membrane encloses the organelle, while the inner membrane folds inward to form cristae, increasing the surface area for energy production. Within the inner membrane lies the mitochondrial matrix, containing enzymes involved in ATP production.
Function: Mitochondria primarily generate ATP through cellular respiration, a process that involves the breakdown of glucose and other molecules to produce energy. This process occurs in several stages:
- Glycolysis: Glucose is broken down into pyruvate in the cytoplasm, producing a small amount of ATP.
- Pyruvate Oxidation: Pyruvate enters the mitochondria and undergoes further oxidation to produce acetyl-CoA, which enters the citric acid cycle.
- Citric Acid Cycle (Krebs Cycle): Acetyl-CoA is further oxidized in the mitochondrial matrix, generating ATP and reducing agents (NADH and FADH2).
- Electron Transport Chain (ETC): NADH and FADH2 donate electrons to the ETC, located in the inner mitochondrial membrane. As electrons pass through the ETC, they drive the pumping of protons across the membrane, creating an electrochemical gradient.
- ATP Synthase: The flow of protons back into the mitochondrial matrix through ATP synthase drives the synthesis of ATP from adenosine diphosphate (ADP) and inorganic phosphate.
Role in Cellular Processes: In addition to energy production, mitochondria play essential roles in other cellular processes, including:
- Regulation of cell death (apoptosis)
- Calcium signaling
- Synthesis of certain molecules, such as heme and steroid hormones
- Modulation of cellular metabolism and oxidative stress response
Causes of Mitochondrial Disease:
Understanding the diverse causes of mitochondrial disease is crucial for accurate diagnosis, genetic counseling, and the development of targeted therapies to mitigate its effects.
Genetic Mutations: Mitochondrial disease is primarily caused by mutations in either nuclear DNA or mitochondrial DNA (mtDNA). These mutations can occur spontaneously or be inherited from one or both parents. Mutations in nuclear DNA affect proteins involved in mitochondrial function, while mutations in mtDNA directly impact mitochondrial structure and function.
Inheritance Patterns: Mitochondrial disease can be inherited through various patterns, depending on whether the mutation affects nuclear DNA or mtDNA:
- Maternal Inheritance: Mutations in mtDNA are usually inherited from the mother. This is because the egg cell contributes the majority of the mitochondria to the developing embryo, while sperm typically contribute very few mitochondria.
- Autosomal Inheritance: Mutations in nuclear DNA follow autosomal inheritance patterns and can be inherited from either parent. They may exhibit autosomal recessive, autosomal dominant, or X-linked inheritance patterns.
De Novo Mutations: In some cases, mitochondrial disease may arise from de novo mutations, meaning they occur spontaneously in an individual with no family history of the condition. These mutations can occur during embryonic development or later in life.
Heteroplasmy: Heteroplasmy refers to the presence of both normal and mutated mtDNA within the same cell or individual. The severity of mitochondrial disease can vary depending on the proportion of mutated mtDNA present in affected tissues. Changes in heteroplasmy levels can occur over time and may influence the progression and severity of the disease.
Environmental Factors: While genetic mutations are the primary cause of mitochondrial disease, environmental factors such as toxins, medications, and oxidative stress can exacerbate mitochondrial dysfunction and contribute to disease progression. Additionally, certain environmental factors may interact with genetic predispositions to increase the risk of developing mitochondrial disease.
Types of Mitochondrial Diseases:
Mitochondrial diseases encompass a broad spectrum of disorders that can affect various organs and systems in the body. These diseases can result from nuclear or mitochondrial DNA mutations, leading to dysfunctional mitochondria. Here are some common types.
Mitochondrial Myopathy: This type of mitochondrial disease primarily affects skeletal muscles, leading to weakness, exercise intolerance, and muscle pain. Symptoms may include difficulty walking, muscle weakness, and fatigue.
Mitochondrial Encephalopathy: Mitochondrial encephalopathy refers to disorders that primarily affect the brain, resulting in neurological symptoms such as seizures, developmental delays, cognitive impairment, and movement disorders.
Leigh Syndrome: Leigh syndrome is a severe neurological disorder that typically begins in infancy or early childhood. It is characterized by progressive neurodegeneration, leading to motor and intellectual disabilities, muscle weakness, and respiratory problems.
Leber’s Hereditary Optic Neuropathy (LHON): LHON is a mitochondrial disease that primarily affects the optic nerve, leading to vision loss, usually in young adulthood. It predominantly affects males and can cause rapid, painless vision deterioration.
Kearns-Sayre Syndrome (KSS): KSS is a rare mitochondrial disorder characterized by the triad of progressive external ophthalmoplegia (weakness or paralysis of the eye muscles), pigmentary retinopathy (abnormal pigmentation in the retina), and heart block (a disruption in the heart’s electrical signals).
Mitochondrial Diabetes: Some mitochondrial diseases can affect pancreatic beta cells, leading to impaired insulin secretion and diabetes mellitus.
Mitochondrial Cardiomyopathy: This type of mitochondrial disease affects the heart muscle, leading to cardiomyopathy, arrhythmias, and heart failure. Symptoms may include shortness of breath, fatigue, and chest pain.
Mitochondrial Depletion Syndrome: This group of disorders is characterized by a significant reduction in mitochondrial DNA content, leading to impaired mitochondrial function and multisystem involvement. Symptoms may vary widely depending on the organs affected.
Symptoms of Mitochondrial Disease:
Mitochondrial disease encompasses a wide range of symptoms that can affect various organs and systems in the body. The severity and specific symptoms can vary depending on the type of mitochondrial disease, the extent of mitochondrial dysfunction, and which tissues are primarily affected. Here are some common symptoms:
Fatigue: Chronic fatigue is a hallmark symptom of mitochondrial disease. Individuals may experience persistent tiredness and lack of energy, even after rest or sleep.
Muscle Weakness: Muscle weakness, often accompanied by exercise intolerance, is a common symptom of mitochondrial disease. It can affect both skeletal muscles (used for movement) and smooth muscles (found in organs such as the digestive tract).
Neurological Symptoms: Mitochondrial disease can manifest as a range of neurological symptoms, including:
- Seizures
- Developmental delays
- Cognitive impairment
- Movement disorders (e.g., ataxia, dystonia)
- Stroke-like episodes
Gastrointestinal Issues: Digestive problems such as constipation, diarrhea, vomiting, and swallowing difficulties may occur due to dysfunction of the smooth muscles in the digestive tract.
Vision and Hearing Problems: Mitochondrial disease can affect the eyes and ears, leading to symptoms such as.
- Vision loss or impairment
- Optic nerve atrophy
- Hearing loss or impairment
Cardiac Symptoms: In some cases, mitochondrial disease can affect the heart, resulting in symptoms such as.
- Cardiomyopathy (enlarged or weakened heart muscle)
- Arrhythmias (irregular heartbeats)
- Heart failure
Respiratory Issues: Respiratory problems, including shortness of breath, difficulty breathing, and respiratory muscle weakness, may occur due to impaired mitochondrial function in the respiratory muscles and/or the respiratory centers in the brainstem.
Endocrine Symptoms: Some individuals with mitochondrial disease may experience endocrine abnormalities, such as diabetes mellitus, thyroid dysfunction, or adrenal insufficiency.
Growth and Developmental Delays: Children with mitochondrial disease may exhibit delays in growth and development, including delayed milestones such as walking and talking.
Multiorgan Involvement: Mitochondrial disease can affect multiple organs and systems simultaneously, leading to a wide range of symptoms and complications that may vary in severity among affected individuals.
Diagnosis of Mitochondrial Disease:
Diagnosing mitochondrial disease can be complex and requires a multidisciplinary approach involving clinical evaluation, laboratory testing, and genetic analysis. Here are the key components of the diagnostic process:
Clinical Evaluation: A thorough medical history and physical examination are essential for identifying symptoms and signs suggestive of mitochondrial disease. Healthcare providers will inquire about symptoms, family history, and any relevant medical conditions.
Laboratory Testing: Various laboratory tests may be performed to assess mitochondrial function and identify biomarkers associated with mitochondrial dysfunction. These tests may include:
- Blood tests: to measure lactate, pyruvate, creatine kinase, and other markers of mitochondrial dysfunction.
- Urine tests: to assess organic acid levels and detect abnormal metabolites.
- Muscle biopsy: to examine mitochondrial structure and function, including histopathological analysis, enzyme assays, and electron microscopy.
Imaging Studies: Imaging studies such as magnetic resonance imaging (MRI), computed tomography (CT), and magnetic resonance spectroscopy (MRS) may be used to assess organ involvement and detect abnormalities in the brain, muscles, heart, and other affected tissues.
Genetic Testing: Genetic analysis plays a crucial role in diagnosing mitochondrial disease. Various techniques may be employed to identify mutations in nuclear DNA and mitochondrial DNA, including:
- Next-generation sequencing (NGS): to analyze nuclear DNA for mutations in genes associated with mitochondrial function.
- Mitochondrial DNA sequencing: to detect mutations in mitochondrial DNA, which are often associated with mitochondrial diseases.
Functional Studies: Functional assays may be conducted to assess mitochondrial function directly. These studies may include:
- Measurement of respiratory chain enzyme activities in tissues or cultured cells.
- Assessment of mitochondrial bioenergetics using techniques such as mitochondrial respirometry and ATP production assays.
Clinical Criteria: In some cases, mitochondrial disease may be diagnosed based on specific clinical criteria established by expert consensus, such as the criteria proposed by the Mitochondrial Medicine Society.
Differential Diagnosis: Mitochondrial disease can mimic other medical conditions, and it’s essential to consider alternative diagnoses. Differential diagnosis may involve ruling out other neuromuscular disorders, metabolic disorders, and genetic syndromes with overlapping features.
Multidisciplinary Evaluation: Given the complexity of mitochondrial disease, diagnosis often requires collaboration among various specialists, including neurologists, geneticists, metabolic specialists, and others.
Treatment Options for Mitochondrial Disease:
While there is currently no cure for mitochondrial disease, treatment aims to manage symptoms, improve quality of life, and address specific complications associated with the condition. Here are some treatment options commonly used for mitochondrial disease:
Supportive Care: Supportive care measures focus on addressing symptoms and providing assistance with daily activities. This may include physical therapy, occupational therapy, speech therapy, and nutritional support to optimize overall function and mobility.
Medications: Certain medications may be prescribed to manage symptoms and complications associated with mitochondrial disease. These may include:
- Antiepileptic drugs to control seizures.
- Supplements such as coenzyme Q10 (CoQ10), thiamine (vitamin B1), riboflavin (vitamin B2), and L-carnitine to support mitochondrial function.
- Symptomatic treatments for pain, gastrointestinal issues, cardiac symptoms, and other specific manifestations of the disease.
Nutritional Support: Optimizing nutrition is crucial for individuals with mitochondrial disease. A balanced diet rich in nutrients, antioxidants, and essential vitamins and minerals can help support mitochondrial function and overall health. In some cases, specialized diets, such as ketogenic or high-fat, low-carbohydrate diets, may be recommended.
Avoidance of Triggers: Individuals with mitochondrial disease may be sensitive to certain environmental triggers, such as exposure to toxins, infections, or extreme temperatures. Avoiding these triggers whenever possible can help minimize symptom exacerbation and disease progression.
Genetic Counseling: Genetic counseling is essential for individuals and families affected by mitochondrial disease. Genetic counselors can provide information about the inheritance pattern, recurrence risks, and family planning options. Preimplantation genetic diagnosis (PGD) and prenatal testing may be available for families at risk of passing on mitochondrial disease to future generations.
Investigational Therapies: Research into potential treatments for mitochondrial disease is ongoing, and several experimental therapies are being explored. These may include:
- Mitochondrial-targeted antioxidants and supplements.
- Gene therapy and mitochondrial replacement techniques to address underlying genetic defects.
- Pharmacological agents targeting mitochondrial dysfunction and oxidative stress.
Symptom Management: Given the diverse range of symptoms associated with mitochondrial disease, a multidisciplinary approach involving various specialists, including neurologists, cardiologists, endocrinologists, and others, may be necessary to manage specific symptoms and complications effectively.
Research and Advances in Mitochondrial Disease:
Here’s a glimpse into some of the exciting research developments in mitochondrial disease for 2024 (based on information available until today, April 25, 2024).
Diagnostic Advancements:
- Web-based Mitochondrial Resource: Researchers have developed a new web-based tool called MSeqDR Quick-Mitome (QM). This allows clinicians to upload and analyze genomic data from patients with suspected mitochondrial disease. QM integrates machine learning to prioritize disease-causing variants in both known and novel genes, potentially aiding in faster and more accurate diagnosis.
- 2. Promising Gene Editing Approaches:
- Mitochondrial DNA Base Editors (mitoBEs): This is a new frontier in gene editing for mitochondrial disease. Researchers are developing microbes that use modified enzymes to correct specific mutations in mitochondrial DNA. This approach holds promise for treating mitochondrial diseases caused by mtDNA mutations.
Focus on Mechanisms of Disease:
- Biological Mechanism for Neurological Disorders and Cancers: A recent study identified a new molecular mechanism involved in neuronal death related to mitochondrial dysfunction. This finding could pave the way for the development of therapies targeting this specific pathway in neurological diseases associated with mitochondrial problems.
Clinical Trials and Collaborative Efforts:
- Importance of International Collaboration: The 8th Mitochondrial Medicine – Therapeutic Development Conference in March 2024 highlighted the crucial role of international collaboration between researchers, clinicians, and the life sciences industry to accelerate the discovery and development of effective treatments for mitochondrial diseases.
- Clinical Trial Consortia: Discussions are ongoing to establish international clinical trial consortia to streamline the testing of promising new therapies for mitochondrial diseases. This would expedite the process of bringing effective treatments to patients.
Myths and Misconceptions about Mitochondrial Disease:
Mitochondrial diseases are complex and can be misunderstood. Here are some common myths and misconceptions surrounding them.
Myth #1: Mitochondrial disease is a childhood disease.
Fact: While some children are diagnosed early, mitochondrial disease can affect people of all ages. Symptoms may appear in infancy, childhood, adulthood, or even later in life.
Myth #2: Everyone with mitochondrial disease has intellectual disability.
Fact: The severity and range of symptoms vary greatly. While some individuals may experience developmental delays or intellectual disability, many others have normal cognitive function.
Myth #3: Mitochondrial disease is always inherited from the mother.
Fact: There are several inheritance patterns for mitochondrial diseases. Mitochondrial DNA mutations are passed down from mother to child, but mutations in nuclear genes, which also play a role, can be inherited from either parent or maybe spontaneous mutations.
Myth #4: There is no treatment for mitochondrial disease.
Fact: While there is no cure, there are various treatment approaches that focus on managing symptoms, improving quality of life, and potentially slowing disease progression. This can include supportive therapies like diet management, exercise programs, and specific vitamins or supplements. Research into new treatments like gene therapy and mitochondrial replacement therapy is ongoing.
Myth #5: Pregnancy is impossible for women with mitochondrial disease.
Fact: Women with mitochondrial disease can have children. However, preconception counseling and planning are crucial to assess potential risks and explore options like a prenatal diagnosis to determine the baby’s genetic status.
FAQs about Mitochondrial Disease:
A1: While there is currently no cure for mitochondrial disease, treatment can help manage symptoms and improve quality of life.
A2: Mitochondrial disease can be inherited from a person’s mother, as mitochondria are passed down through the maternal line.
A3: Long-term complications of mitochondrial disease can vary depending on the specific type and severity of the condition but may include neurological issues, muscle weakness, and organ dysfunction.
A4: Mitochondrial disease is considered rare, but its exact prevalence is difficult to determine due to challenges in diagnosis and varying clinical presentations.
A5: If you suspect mitochondrial disease, it’s essential to consult with a healthcare provider who can conduct appropriate testing and provide guidance on management and treatment options.
-Please remember, to always consult with healthcare professionals or Doctors for personalised advice related to medical conditions.
Conclusion:
In conclusion, mitochondrial disease encompasses a diverse group of disorders stemming from dysfunction in the mitochondria, the cell’s energy-producing organelles. It can affect various organs and systems, with symptoms ranging from fatigue and muscle weakness to neurological and gastrointestinal issues. Diagnosis involves a multidisciplinary approach, including clinical evaluation, genetic testing, and functional studies. While there is no cure, treatment focuses on symptom management, supportive care, and experimental therapies. Ongoing research holds promise for advancements in diagnosis and treatment, emphasizing the importance of international collaboration and genetic counseling.




