
HEALTH BLOG
What Is Mucositis And What Are Its Causes, Symptoms, And Treatment Options
-
 Rahul Priydarss
Rahul Priydarss - March 5, 2024
Learn about mucositis its causes, symptoms, and treatment options. Understand how chemotherapy, radiation therapy, infections, and medications can trigger mucositis. Discover prevention strategies, home remedies, and ongoing research to manage this common side effect of cancer treatment.
Introduction to Mucositis:
Mucositis is a common and often painful condition characterized by inflammation and ulceration of the mucous membranes lining the digestive tract. These membranes include those found in the mouth, throat, esophagus, and gastrointestinal tract. Mucositis can be a side effect of cancer treatment, particularly chemotherapy and radiation therapy, but it can also occur due to other causes such as infections or autoimmune diseases.
The condition occurs because chemotherapy and radiation therapy not only target cancer cells but also affect rapidly dividing healthy cells, including those in the mucous membranes. This damage leads to inflammation, erosion, and ulceration of the mucosal lining, which can result in symptoms such as pain, difficulty swallowing, dry mouth, mouth sores, and increased susceptibility to infections.

Table of Contents
What is Mucositis:
Mucositis is a condition characterized by inflammation and ulceration of the mucous membranes lining the digestive tract, particularly the mouth and throat. It is a common side effect of certain medical treatments, such as chemotherapy and radiation therapy for cancer, as well as some types of medication. Symptoms of mucositis may include pain, redness, swelling, and difficulty swallowing. Treatment typically focuses on managing symptoms and preventing complications, such as infection.
Causes of Mucositis:
Chemotherapy: Chemotherapy drugs are designed to kill rapidly dividing cancer cells. Unfortunately, they can also affect other rapidly dividing cells in the body, including the cells that line the digestive tract. As a result, the mucous membranes in the mouth, throat, esophagus, stomach, and intestines can become inflamed and ulcerated, leading to mucositis.
Radiation therapy: Radiation therapy uses high-energy beams to target and destroy cancer cells. Radiation directed at tumors in the head and neck region can inadvertently damage healthy cells in the surrounding tissues, including the mucous membranes. This damage can cause inflammation and ulceration, resulting in mucositis.
Stem cell transplantation: Stem cell transplantation, also known as bone marrow transplantation, is a procedure used to treat certain cancers and other diseases. High-dose chemotherapy and/or radiation therapy are often administered before the transplant to destroy cancer cells and suppress the immune system. This can damage the mucous membranes, leading to mucositis.
Infections: Infections in the mouth or throat, such as oral thrush (a fungal infection), herpes simplex virus (cold sores), or bacterial infections, can irritate the mucous membranes and contribute to the development of mucositis. Individuals with weakened immune systems, such as those undergoing cancer treatment, are particularly susceptible to these infections.
Certain medications: Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics, may irritate the mucous membranes and increase the risk of developing mucositis. This is especially true if these medications are taken for an extended period or at high doses.
Poor oral hygiene: Inadequate oral hygiene practices, such as infrequent brushing and flossing, can increase the risk of developing mucositis.
Tobacco and alcohol use: Smoking tobacco and excessive alcohol consumption can irritate the mucous membranes and increase the risk of mucositis, especially in the oral cavity.
Pre-existing oral conditions: Conditions such as gingivitis, periodontal disease, and oral thrush can predispose individuals to developing mucositis.
Certain medications: Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can cause mucosal irritation and contribute to the development of mucositis.
Symptoms of Mucositis:
Various symptoms show the infection or severity of mucositis.
Pain or discomfort: Mucositis often causes varying degrees of pain or discomfort, ranging from mild irritation to severe soreness. This discomfort can affect the mouth, throat, and other parts of the digestive tract. Eating, drinking, and talking may exacerbate the pain.
Redness and inflammation: The affected mucous membranes may appear red, swollen, and inflamed. This inflammation is a result of the body’s immune response to the damage caused by chemotherapy, radiation therapy, infections, or other triggers.
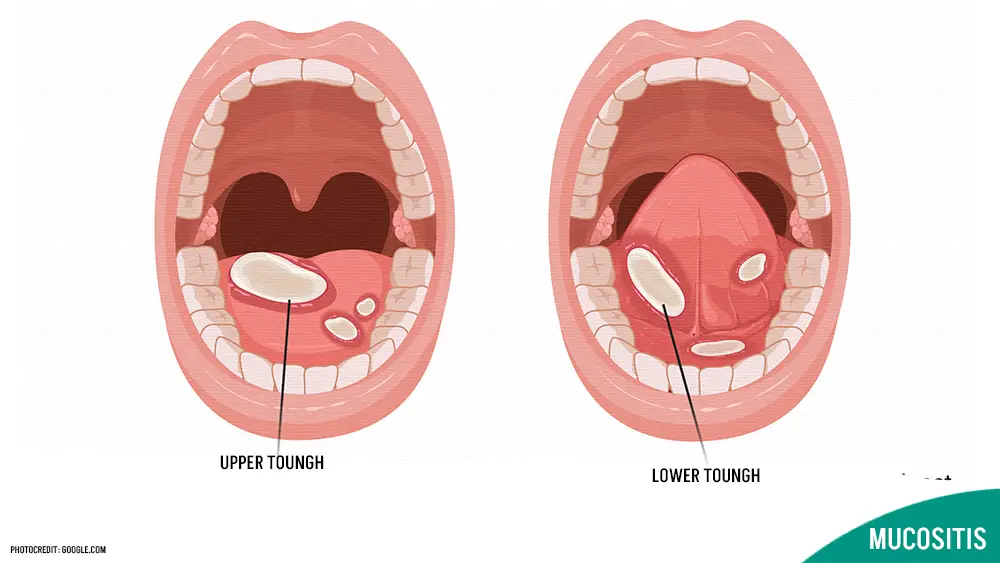
Ulcers or sores: Mucositis can lead to the development of ulcers or sores in the mouth, throat, or gastrointestinal tract. These ulcers may vary in size and severity, and they can be painful, making it uncomfortable to eat, drink, or swallow.
Difficulty swallowing (dysphagia): Inflammation, ulcers, or pain in the throat or esophagus can make swallowing difficult or painful. This can lead to reluctance to eat or drink, which may result in dehydration and malnutrition if left untreated.
Dry mouth (xerostomia): Mucositis can decrease saliva production, leading to a dry mouth sensation. Saliva helps moisten and cleanse the mouth, so a decrease in saliva can exacerbate discomfort and increase the risk of oral infections.
Changes in taste: Some individuals with mucositis may experience alterations in taste perception, such as a metallic or bitter taste in the mouth. Changes in taste can further reduce appetite and enjoyment of food, leading to decreased nutritional intake.
Bad breath (halitosis): The combination of decreased saliva, oral inflammation, and the presence of ulcers or sores can contribute to bad breath. Maintaining good oral hygiene practices, such as regular brushing and flossing, can help manage halitosis.
Increased risk of infection: Mucositis can compromise the integrity of the mucous membranes, making them more susceptible to infection by bacteria, viruses, or fungi. Infections in the mouth, throat, or gastrointestinal tract can further exacerbate symptoms and delay healing.
Types of Mucositis:
Mucositis can be categorized into several types based on the location and underlying cause of the inflammation. Some common types of mucositis include.
Oral mucositis: This type of mucositis affects the mucous membranes lining the mouth, including the gums, tongue, cheeks, and palate. It is commonly associated with chemotherapy and radiation therapy for head and neck cancer, as well as certain medications and infections.
Gastrointestinal mucositis: This type of mucositis affects the mucous membranes lining the digestive tract, including the esophagus, stomach, and intestines. It can cause symptoms such as abdominal pain, nausea, vomiting, diarrhea, and difficulty swallowing. Gastrointestinal mucositis is often seen in cancer patients undergoing chemotherapy or radiation therapy, as well as those receiving high-dose chemotherapy before stem cell transplantation.
Genitourinary mucositis: This type of mucositis affects the mucous membranes of the urinary and genital tracts. It can cause symptoms such as pain or discomfort during urination, urinary frequency or urgency, vaginal dryness or irritation, and painful intercourse. Genitourinary mucositis can occur as a side effect of radiation therapy or chemotherapy for pelvic cancers, as well as certain infections.
Ocular mucositis: This type of mucositis affects the mucous membranes of the eyes, including the conjunctiva (the thin, transparent membrane covering the white part of the eye) and the cornea (the clear, dome-shaped surface that covers the iris and pupil). It can cause symptoms such as redness, irritation, tearing, and sensitivity to light. Ocular mucositis can occur as a side effect of radiation therapy or chemotherapy for head and neck cancers, as well as certain autoimmune conditions.
Diagnosis of Mucositis:
Diagnosing mucositis typically involves a combination of clinical evaluation, physical examination, and medical history review. Here’s an overview of the diagnostic process.
Clinical evaluation: Healthcare providers will assess the patient’s symptoms, including any pain, discomfort, difficulty swallowing, or other signs of mucositis. They may ask about the timing of symptom onset, any treatments the patient has undergone (such as chemotherapy or radiation therapy), and any underlying medical conditions.
Physical examination: A thorough examination of the oral cavity, throat, and gastrointestinal tract may be performed to look for signs of inflammation, ulceration, or infection. This may involve using a lighted instrument to visualize the inside of the mouth and throat and palpating (feeling) the tissues for abnormalities.
Medical history review: Healthcare providers will review the patient’s medical history, including any previous episodes of mucositis, underlying medical conditions, medications, and treatments. This information can help identify potential triggers or risk factors for mucositis.
Biopsy: In some cases, a biopsy may be performed to obtain a small tissue sample from the affected area for further examination under a microscope. A biopsy can help confirm the diagnosis of mucositis and rule out other conditions, such as oral cancer or fungal infections.
Laboratory tests: Blood tests may be ordered to assess for signs of infection or inflammation, as well as to evaluate the patient’s overall health status. This may include a complete blood count (CBC), inflammatory markers, and tests for specific pathogens, depending on the suspected cause of mucositis.
Prevention From Mucositis:
Prevention of mucositis can be challenging, but some strategies may help reduce the risk or severity of the condition.
Oral care: Maintaining good oral hygiene is crucial in preventing mucositis. This includes brushing teeth gently with a soft-bristled toothbrush and fluoride toothpaste, flossing daily, and rinsing the mouth with a saline solution or prescribed mouthwash. Regular dental check-ups can also help identify and address any dental issues that may contribute to mucositis.
Care during cancer treatment: For individuals undergoing chemotherapy or radiation therapy, supportive care measures such as cryotherapy (ice therapy) or oral rinses with saline or bicarbonate solution may help reduce the severity of mucositis. These interventions should be discussed with a healthcare provider.
Dietary modifications: Eating a soft, bland diet and avoiding spicy, acidic, or rough-textured foods can help minimize irritation to the mucous membranes during cancer treatment. It’s also important to stay hydrated by drinking plenty of fluids, preferably water, to maintain moisture in the mouth and throat.
Medications: In some cases, medications such as oral mucosal protectants (e.g., sucralfate) or topical analgesics (e.g., lidocaine gel) may be prescribed to help alleviate pain and discomfort associated with mucositis. These medications should be used under the guidance of a healthcare provider.
Radiation therapy techniques: Advanced radiation therapy techniques, such as intensity-modulated radiation therapy (IMRT) or proton therapy, may help minimize radiation exposure to healthy tissues and reduce the risk of mucositis. These techniques should be discussed with a radiation oncologist.
Avoidance of known triggers: Individuals who are prone to mucositis should avoid known triggers such as smoking, alcohol consumption, and certain medications that may exacerbate the condition. It’s important to discuss any potential risk factors with a healthcare provider.
Regular monitoring: Close monitoring of oral health and mucosal integrity during cancer treatment can help detect mucositis early and allow for timely intervention. Healthcare providers should conduct regular assessments and provide appropriate support and management strategies as needed.
Treatment Options for Mucositis:
Treatment options for mucositis aim to manage symptoms, promote healing, and prevent complications. Some common approaches include.
Pain management: Over-the-counter pain relievers such as acetaminophen, aceclofenac, diclofenac or ibuprofen may help alleviate discomfort associated with mucositis. Prescription medications, such as topical anesthetics or oral rinses(Ora-T, Hexadine, Listrine) containing lidocaine or any other local anaesthetics, may also be recommended for more severe pain.
Topical oral care: Gentle oral hygiene practices, such as brushing with Glister Toothpaste a soft toothbrush and using alcohol-free mouthwashes, can help maintain oral health and reduce the risk of infection. Avoiding alcohol-based mouthwashes and abrasive toothpaste is important to prevent further irritation.
Moisturizing agents: Oral moisturizing agents, such as artificial saliva or saliva substitutes, can help alleviate dry mouth and provide relief from discomfort. These products help lubricate the oral tissues and promote healing.
Nutritional support: Maintaining adequate nutrition is essential for managing mucositis and supporting overall health. In cases where eating solid foods is difficult, consuming soft or liquid foods and beverages, such as smoothies, soups, and nutritional supplements, can help meet nutritional needs. In severe cases, a feeding tube may be necessary to ensure adequate nutrition.
Medications: Depending on the severity of mucositis, healthcare providers may prescribe medications to reduce inflammation, control pain, or prevent infection. These may include corticosteroids, oral rinses containing antifungal or antibacterial agents, or prescription-strength pain relievers with antifungal medicine line fluconazole, and albendazole.
Cryotherapy: Cryotherapy, or cooling of the oral cavity, has been shown to reduce the severity of mucositis in some cancer patients undergoing chemotherapy. Cooling the mouth with ice chips or a cold pack during chemotherapy infusion may help minimize damage to the mucous membranes and decrease the risk of developing mucositis.
Supportive care: Emotional support and counseling can be valuable components of mucositis treatment, as coping with the physical and emotional effects of the condition can be challenging. Support groups, counseling services, and resources provided by healthcare providers can help patients and their caregivers navigate the treatment process and maintain overall well-being.
Home Remedies for Mucositis:
Here are some home remedies that may help alleviate the symptoms of mucositis.
Maintain good oral hygiene: Brush your teeth gently with a soft-bristled toothbrush after meals and before bedtime. Use alcohol-free mouthwash or saline solution to rinse your mouth several times a day to keep it clean and prevent infection.
Stay hydrated: Drink plenty of fluids, such as water, herbal teas, or clear broths, to keep your mouth and throat moist and prevent dehydration. Avoid acidic or spicy foods and beverages that can irritate the mucous membranes.
Use soothing mouth rinses: Rinse your mouth with a solution of baking soda and water (1 teaspoon of baking soda in 1 cup of warm water) or a mixture of salt and water (1/2 teaspoon of salt in 1 cup of warm water) to help soothe soreness and reduce inflammation.
Avoid irritating foods: Avoid spicy, acidic, or rough-textured foods that can further irritate the mucous membranes and exacerbate symptoms. Opt for soft, bland foods that are easy to swallow, such as mashed potatoes, yogurt, oatmeal, or smoothies.
Stay away from tobacco and alcohol: Smoking and alcohol can irritate the mucous membranes and delay healing. Avoid tobacco products and limit alcohol consumption to promote faster recovery.
Use a humidifier: If the air in your home is dry, using a humidifier can help moisten the air and alleviate dry mouth and throat symptoms. Be sure to clean the humidifier regularly to prevent the growth of bacteria or mold.
Eat smaller, more frequent meals: If swallowing is painful, try eating smaller, more frequent meals throughout the day instead of larger meals. This can help prevent fatigue and reduce the risk of dehydration and malnutrition.
Research and Developments for Mucositis:
Research and developments for mucositis are focused on various aspects, including prevention, treatment, and management of symptoms. Some of the key areas of research and development include.
Prevention strategies: Researchers are investigating ways to prevent or minimize the development of mucositis in individuals undergoing cancer treatment or other therapies known to cause mucositis. This includes studying the use of oral care protocols, cryotherapy (cooling treatments), and mucosal protective agents before and during treatment.
Novel treatments: Scientists are exploring new therapeutic approaches for mucositis, such as topical agents, mouthwashes, gels, or oral rinses containing anti-inflammatory, analgesic, or mucosal protective properties. These treatments aim to reduce inflammation, alleviate pain, promote healing, and prevent infections.
Targeted therapies: Researchers are investigating targeted therapies that specifically target the molecular pathways involved in the development and progression of mucositis. This includes studying the use of growth factors, cytokine inhibitors, and other biological agents to modulate the inflammatory response and promote tissue repair.
FAQs about Mucositis:
A1: Main symptoms include pain, difficulty swallowing, and increased risk of infection.
A2: While it may not always be preventable, certain strategies such as good oral hygiene and medication adjustments can help reduce the risk of mucositis.
A3: Treatment options include pain management, topical treatments, nutritional support, and management of potential complications.
A4: Long-term effects may include scarring, changes in taste sensation, and emotional distress.
A5: Some alternative treatments such as acupuncture, herbal remedies, and dietary supplements may provide relief from mucositis symptoms, but more research is needed to confirm their effectiveness.

-Please remember, to always consult with healthcare professionals or Doctors for personalised advice related to medical conditions.
Conclusion:
Mucositis is a common complication of cancer treatment that can cause pain, discomfort, and difficulty swallowing. Early detection and management of mucositis are essential for minimizing symptoms and improving the quality of life for patients undergoing cancer treatment. By implementing preventive measures, exploring new treatment options, and providing supportive care services, healthcare providers can help patients cope with the challenges of mucositis and improve their overall well-being.




