
HEALTH BLOG
What Is Rubella and Their Causes, Symptoms, and Prevention
-
Rahul Priydarss
This article details study about all you need to know about Rubella, also known as German measles, in this comprehensive guide. Learn about the symptoms, causes, diagnosis, treatment options, and prevention strategies for Rubella. Stay informed and protect yourself and your loved ones from this contagious viral infection. Read on now!”
What Is Rubella:
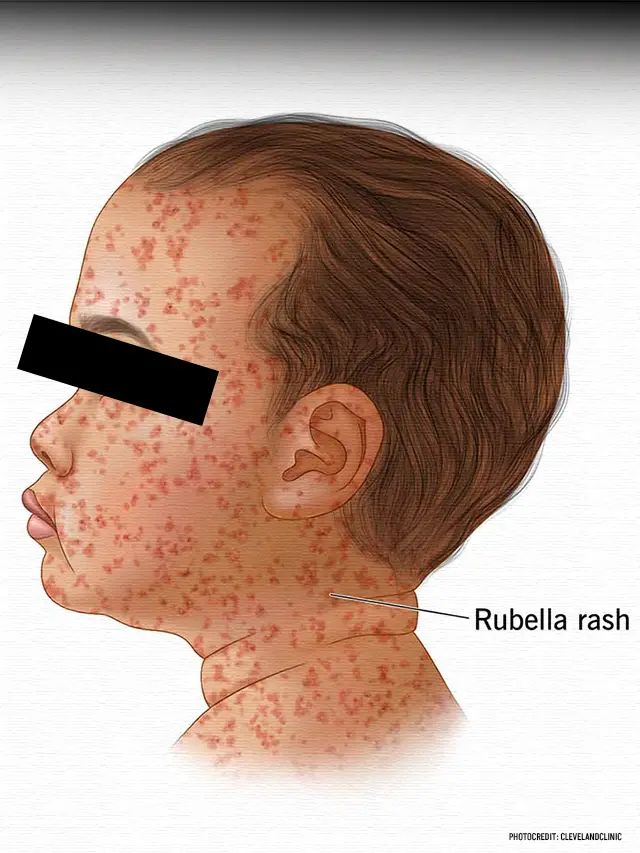
Rubella, also known as German measles, is a contagious viral infection characterized by a distinctive red rash. While often milder than measles, rubella can still pose serious risks, particularly to pregnant women and their unborn babies. Understanding the causes, symptoms, complications, and prevention strategies associated with rubella is essential for effective management and control of the disease.

Table of Contents
Rubella Caused By:
Rubella is caused by the rubella virus, which is transmitted from person to person through respiratory droplets. Close contact with an infected individual, such as being in the same room or sharing utensils, can facilitate the spread of the virus. Rubella is most contagious when the infected person has a rash, but transmission can also occur in the days leading up to the onset of the rash.
Symptoms of Rubella:
The hallmark symptom of rubella is a red rash that typically begins on the face and then spreads to the rest of the body. Other common symptoms include fever, headache, sore throat, swollen lymph nodes, and a runny or stuffy nose. In some cases, particularly in children, rubella may present with mild or no symptoms at all, making diagnosis more challenging.
Is a viral infection that often causes mild symptoms, but it can be dangerous for pregnant women and their babies. Here are the common symptoms of rubella.
- Rash: One of the most recognisable symptoms of rubella is a pink or light red rash that typically starts on the face and then spreads to the rest of the body. The rash usually lasts for a few days.
- Fever: People with rubella often develop a mild fever, usually ranging from 99 to 100.5 degrees Fahrenheit (37.2 to 38.1 degrees Celsius).
- Lymphadenopathy: This refers to swelling of the lymph nodes, particularly those located behind the ears and at the back of the head.
- Headache: Many individuals with rubella experience headaches, which can range from mild to moderate in intensity.
- Runny or stuffy nose: Some people may also have symptoms similar to a cold, including a runny or congested nose.
- Conjunctivitis: Rubella can cause redness and inflammation of the eyes, known as conjunctivitis or “pink eye.”
- General discomfort: Individuals with rubella may feel generally unwell, with symptoms such as fatigue and discomfort.
Complications with Rubella:
While rubella is usually a mild illness, it can lead to serious complications, especially in certain populations. Pregnant women who contract rubella are at risk of miscarriage, stillbirth, or giving birth to a baby with congenital rubella syndrome (CRS), which can cause severe birth defects such as deafness, blindness, heart defects, and developmental delays.
Diagnosis of Rubella:
Rubella is diagnosed based on clinical symptoms and confirmed through laboratory testing, such as a blood test to detect the presence of rubella antibodies. In some cases, a throat swab or nasal swab may be taken to test for the presence of the virus itself.

Treatment of Rubella:
There is no specific treatment for rubella, as it is a viral infection that typically resolves on its own within a week to ten days. Treatment focuses on relieving symptoms, such as fever and discomfort, through rest, hydration, and over-the-counter medications like acetaminophen or ibuprofen. It is essential to avoid contact with others, especially pregnant women until the rash has disappeared to prevent further spread of the virus.
Rubella in Pregnancy:
Pregnant women who are not immune to rubella should avoid contact with anyone who has the infection to reduce the risk of complications. If a pregnant woman is exposed to rubella, she should consult her healthcare provider immediately to determine the appropriate course of action, which may include testing for immunity, monitoring for symptoms, and considering post-exposure prophylaxis.
Rubella treatment in Pregnancy:
Treatment for rubella during pregnancy primarily focuses on managing symptoms and preventing complications. However, there is no specific antiviral medication to treat rubella itself. Instead, healthcare providers typically recommend:
- Rest and hydration: Adequate rest and staying hydrated can help the body fight off the infection and alleviate symptoms.
- Fever management: Acetaminophen (Tylenol) may be recommended to reduce fever. However, pregnant women should consult their healthcare provider before taking any medication.
- Monitoring for complications: Regular monitoring by healthcare providers is essential to detect any potential complications, such as fetal abnormalities or signs of CRS.
- Preventive measures: Pregnant women who are not immune to rubella should avoid close contact with individuals who have the infection. Additionally, vaccination against rubella is not recommended during pregnancy, but women should ensure they are up-to-date on vaccinations before becoming pregnant to prevent rubella infection.
- Consultation with a specialist: In cases where rubella infection occurs during pregnancy, healthcare providers may refer the woman to a maternal-fetal medicine specialist or other relevant specialists for additional monitoring and management.
Rubella Outbreaks:
Rubella outbreaks can occur in communities with low vaccination rates or in populations with inadequate access to healthcare. Prompt identification and containment of outbreaks are essential to prevent further spread of the virus and protect vulnerable individuals, particularly pregnant women and their unborn babies.
Rubella vs. Measles: Key Differences:
While rubella and measles are both viral infections that can cause a red rash, they are caused by different viruses and have distinct clinical features. Rubella is typically milder than measles and is characterized by a shorter duration of illness and less severe complications. However, both diseases can be prevented through vaccination and pose risks to vulnerable populations.
The Global Impact of Rubella:
Rubella remains a public health concern globally, particularly in regions with limited access to healthcare and vaccination services. Efforts to improve vaccination coverage, strengthen surveillance systems, and enhance public awareness about the importance of rubella vaccination are essential for achieving the goal of rubella elimination and preventing the devastating consequences of congenital rubella syndrome.
FAQs about Rubella
A1: Rubella infection typically resolves without long-term effects in most cases. However, if rubella occurs during pregnancy, it can lead to serious complications for the unborn baby, known as congenital rubella syndrome (CRS). CRS can cause permanent disabilities such as deafness, blindness, heart defects, and developmental delays.
A2: Yes, adults who were not vaccinated against rubella as children can still contract the virus if they come into contact with an infected person. Rubella is highly contagious, and adults who have not been vaccinated may be at risk of infection, particularly in settings where the virus is circulating.
A3: No, rubella and measles are caused by different viruses and have distinct clinical features. Rubella, also known as German measles, typically causes a milder illness characterized by a red rash, low-grade fever, and mild respiratory symptoms. Measles, on the other hand, is a more severe illness characterized by a high fever, cough, runny nose, red eyes, and a widespread rash.
A4: The rubella vaccine provides long-lasting immunity in most cases. Studies have shown that immunity to rubella persists for at least 15-20 years after vaccination, and in many cases, it may last a lifetime. However, some individuals may experience waning immunity over time, particularly as they age.
A5: If a pregnant woman is exposed to rubella, she needs to consult her healthcare provider immediately. Depending on her immune status and the timing of exposure, the healthcare provider may recommend testing for immunity, monitoring for symptoms of rubella infection, and considering post-exposure prophylaxis with immune globulin (IG) to reduce the risk of congenital rubella syndrome (CRS) in the unborn baby. Early intervention and appropriate medical management are crucial to minimizing the risk of complications for both the pregnant woman and her baby.
modifications, and in some cases, surgical interventions.
-Please remember, to always consult with healthcare professionals or Doctors for personalised advice related to medical conditions.
Conclusion:
Rubella is a contagious viral infection that can cause a red rash, fever, and other symptoms, with potentially serious complications, especially for pregnant women and their unborn babies. Vaccination is the most effective way to prevent rubella and its complications, highlighting the importance of maintaining high vaccination coverage rates and supporting immunization efforts globally.




