You’ll learn how to detect it early and why regular hCG monitoring after pregnancy is crucial. Written with expert insight and personal experience, this article offers reliable, medically sound advice on navigating GTD effectively. Whether you’re recovering from pregnancy or supporting someone who is, this guide offers everything you need to know in a clear, helpful format.
Understanding When GTD Happens:
If you’ve recently had a pregnancy and are experiencing unusual symptoms like heavy vaginal bleeding or persistent high hCG levels, you might have come across the term Gestational Trophoblastic Disease (GTD). As someone who has seen patients go through the ups and downs of this rare condition, I understand how confusing and frightening it can feel at first. GTD refers to a group of rare tumors that involve abnormal growth of cells inside a woman’s uterus cells that should normally form the placenta during pregnancy.
Although GTD is rare, it’s essential to know when it can occur, especially if you’ve had a molar pregnancy or an abnormal miscarriage. Recognizing the timing and risk factors early is key to proper diagnosis and treatment. In this guide, we’ll break down everything you need to know in plain language when it happens, why it happens, and what to watch out for. We’ll also look at expert-backed facts using the latest medical insights to ensure you’re getting trustworthy, helpful information.
GTD usually appears within weeks to months after pregnancy but should always be monitored with follow-up hCG tests.
When Does Gestational Trophoblastic Disease Occur:
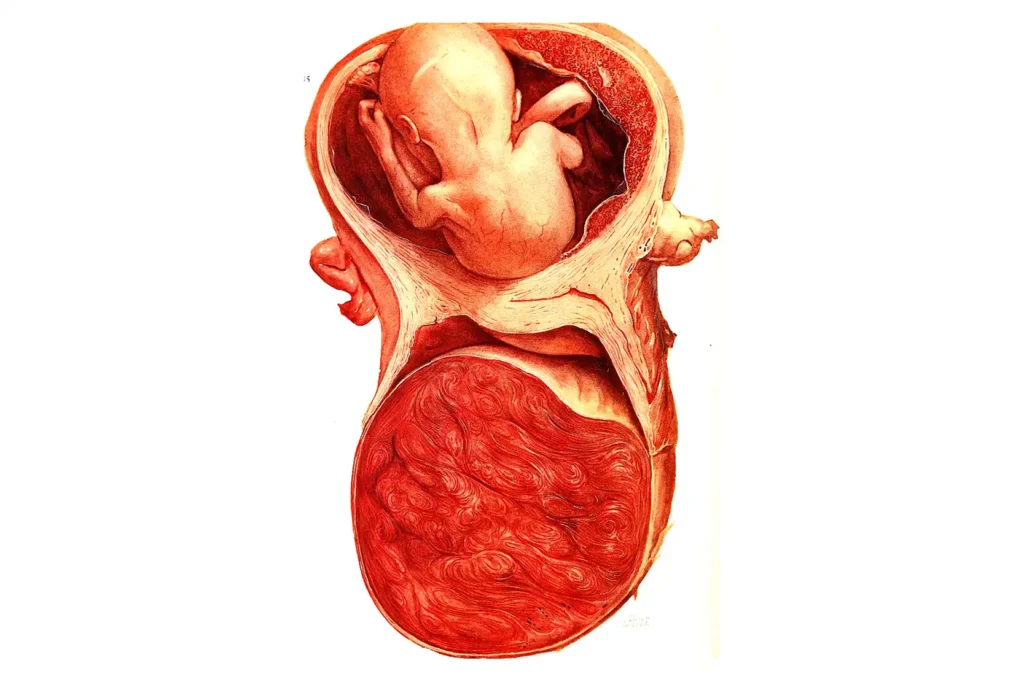
GTD can occur during any stage of pregnancy but most frequently develops after a molar pregnancy, which is a type of non-viable pregnancy where a mass of cysts grows instead of a healthy placenta. It can also develop after a miscarriage, abortion, ectopic pregnancy, or even full-term delivery. The majority of cases are diagnosed within a few weeks to a few months after the pregnancy ends.
One reason GTD can be tricky is because it doesn’t always show up right away. Sometimes, women may think the pregnancy is over, but the abnormal trophoblastic tissue remains and begins to grow uncontrollably. This growth leads to persistently high levels of the pregnancy hormone hCG, even after pregnancy has ended. These levels help doctors suspect GTD and begin investigations.
Causes and Risk Factors for GTD:
The exact cause of GTD isn’t always clear, but it’s closely linked to genetic problems during fertilization. For example, in a complete molar pregnancy, the sperm fertilizes an empty egg, resulting in abnormal cell growth. In a partial mole, two sperm fertilize a normal egg, causing abnormal tissue formation.
Women under 20 or over 40 have a higher risk of developing GTD. A previous molar pregnancy also significantly increases your risk. Other risk factors include nutritional deficiencies and living in certain geographic regions where molar pregnancies are more common, such as parts of Asia and Latin America.
How Is GTD Diagnosed and Detected:
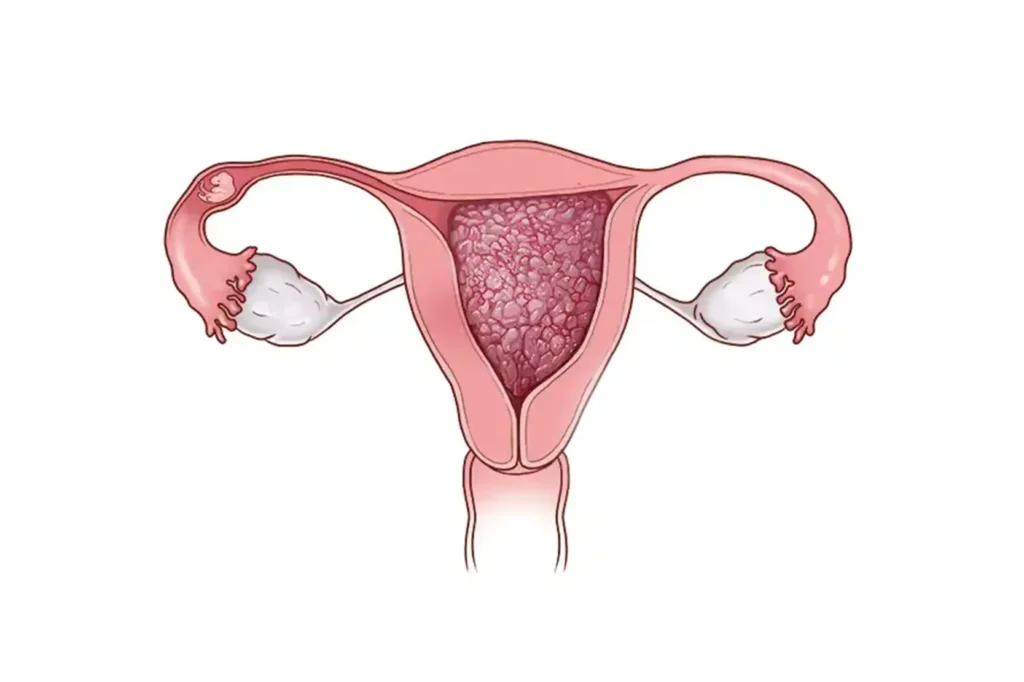
GTD is often diagnosed after pregnancy through unusual symptoms or routine follow-up hCG blood tests. Persistently high or rising hCG levels after a pregnancy event are often the first red flag. Your healthcare provider might also order a pelvic ultrasound, which can reveal abnormal tissue in the uterus.
In some cases, GTD is found during dilation and curettage (D&C) for suspected miscarriage. Once diagnosed, the specific type of GTD (such as invasive mole or choriocarcinoma) will determine your treatment approach and follow-up schedule.
Common Symptoms of GTD:
Many symptoms of GTD mimic those of normal pregnancy or miscarriage, which can make it tricky to detect early. Some types of GTD, especially malignant forms like choriocarcinoma, can metastasize (spread) to other parts of the body such as lungs or brain, leading to symptoms like coughing up blood or neurological changes.
- Abnormal or heavy vaginal bleeding
- Uterine enlargement that’s inconsistent with gestational age
- Severe nausea and vomiting (hyperemesis)
- Pelvic pain or pressure
- Very high levels of hCG without a viable pregnancy
Treatment Options and Prognosis:
The good news is that GTD is highly treatable, especially when detected early. Most benign forms, such as hydatidiform moles, are removed through D&C. After surgery, patients undergo regular hCG monitoring to ensure all molar tissue has been eliminated.
If the disease has spread or is malignant, chemotherapy is often effective. Drugs like methotrexate or actinomycin-D are commonly used. In rare, resistant cases, a combination of therapies may be required. The prognosis for most patients is excellent with cure rates nearing 100% for non-metastatic cases.
Personal Experience and Medical Insight:
As a medical professional who has guided many patients through GTD diagnosis and treatment, I cannot stress enough the importance of regular follow-up after any kind of pregnancy event, especially molar pregnancy. GTD can sneak up silently, but with proper hCG monitoring and early detection, it’s manageable and treatable.
If you’re going through this, know that you’re not alone and there’s a clear path forward. Trust your body, stay informed, and work closely with your healthcare team.
FAQ
Most frequent questions and answers
Yes, although rare, GTD can develop after a full-term delivery due to retained abnormal placental tissue.
Not always. Some types, like hydatidiform moles, are benign, while others like choriocarcinoma are malignant but highly treatable.
GTD usually appears within weeks to months after pregnancy but should always be monitored with follow-up hCG tests.
Conclusion:
Understanding when does Gestational Trophoblastic Disease occur is vital for early detection and treatment. This condition most often arises after a molar pregnancy, miscarriage, or even a normal delivery. Recognizing the symptoms and monitoring hCG levels after any pregnancy event can lead to timely diagnosis. With today’s medical advances, GTD is highly treatable, especially when caught early. If you’ve experienced any type of pregnancy loss or complications, consult your doctor and stay proactive about your reproductive health.