NEUROSCIENCE
Epilepsy: Types, Causes, Symptoms, Treatment and Raising Awareness
-
Rahul Priydarss
Explore the complexities of epilepsy with our comprehensive guide. Learn about its definition, causes, diagnosis, treatment options, and living with the condition. Discover various seizure types and the importance of raising awareness through education, social media, events, and advocacy efforts. Join us in promoting understanding and support for individuals affected by epilepsy. Read more now.
Introduction Of Epilepsy:
In essence, epilepsy is a complex neurological condition that warrants attention and understanding from both healthcare professionals and the broader community. By recognizing its significance and working together to increase awareness and knowledge, we can empower those living with epilepsy and promote a more inclusive and supportive society.
Definition and Overview Of Epilepsy:
Epilepsy is a neurological disorder characterized by recurrent seizures, which are sudden, uncontrolled electrical disturbances in the brain. These seizures can manifest in various forms, from brief lapses of consciousness to convulsions and loss of motor control. It affects people of all ages, backgrounds, and walks of life, with approximately 50 million individuals worldwide diagnosed with epilepsy.
Importance of Understanding Epilepsy:
Understanding epilepsy is crucial due to its significant impact on individuals’ lives and society as a whole. By gaining insight into the causes, symptoms, and management of epilepsy, we can better support those living with the condition and improve their quality of life. Furthermore, awareness and knowledge about epilepsy help reduce stigma and discrimination faced by individuals with the disorder, fostering a more inclusive and supportive environment.
Table of Contents
Types of Epilepsy:
Epilepsy encompasses various types of seizures, each with distinct characteristics and manifestations. Understanding these different seizure types is crucial for accurate diagnosis and appropriate management. Here are some common types of epilepsy seizures.
1- Generalized Seizures:
- Tonic-Clonic Seizures (formerly known as Grand Mal): These seizures involve loss of consciousness, stiffening of muscles (tonic phase), followed by jerking and convulsions (clonic phase). They can cause bodily injuries and may last for a few minutes.
- Absence Seizures (formerly known as Petit Mal): Absence seizures cause brief lapses of consciousness, where the individual appears to be staring blankly into space. They often last for just a few seconds and may go unnoticed.
- Myoclonic Seizures: These seizures involve sudden, brief muscle jerks or twitches, which may affect specific body parts or the entire body.
- Atonic Seizures: Also known as drop attacks, atonic seizures cause a sudden loss of muscle tone, leading to a collapse or fall.
2- Partial (Focal) Seizures:
- Simple Partial Seizures: These seizures do not cause loss of consciousness. They may involve involuntary movements, sensory changes, or emotions.
- Complex Partial Seizures: Complex partial seizures typically alter consciousness and may cause repetitive movements, automatic behaviors, or unusual sensations.
- Secondarily Generalized Seizures: Partial seizures that spread to involve both hemispheres of the brain, resulting in generalized symptoms like convulsions or loss of consciousness.
3- Other Seizure Types:
- Febrile Seizures: These seizures occur in young children during fevers and are usually harmless.
- Psychogenic Non-Epileptic Seizures (PNES): PNES resemble epileptic seizures but are not caused by abnormal brain activity. They often stem from psychological factors.
4- Status Epilepticus: Status epilepticus refers to prolonged seizures or a series of seizures occurring without recovery between them. It is a medical emergency requiring immediate intervention to prevent serious complications.
Causes of Epilepsy:
Epilepsy can arise from various underlying causes, often stemming from abnormalities in the brain’s electrical activity. While the exact cause of epilepsy may not always be clear, several factors can contribute to its development.
Genetic Factors: Genetic predisposition plays a significant role in some cases of epilepsy. Individuals with a family history of epilepsy are at a higher risk of developing the condition.
Brain Trauma or Injury: Head injuries resulting from accidents, falls, or trauma can lead to epilepsy. Damage to the brain tissue can disrupt normal electrical activity and trigger seizures.
Brain Conditions: Certain brain conditions or structural abnormalities can increase the likelihood of epilepsy. These may include tumors, strokes, brain infections (such as meningitis or encephalitis), developmental disorders (like cerebral palsy), or malformations of brain development.
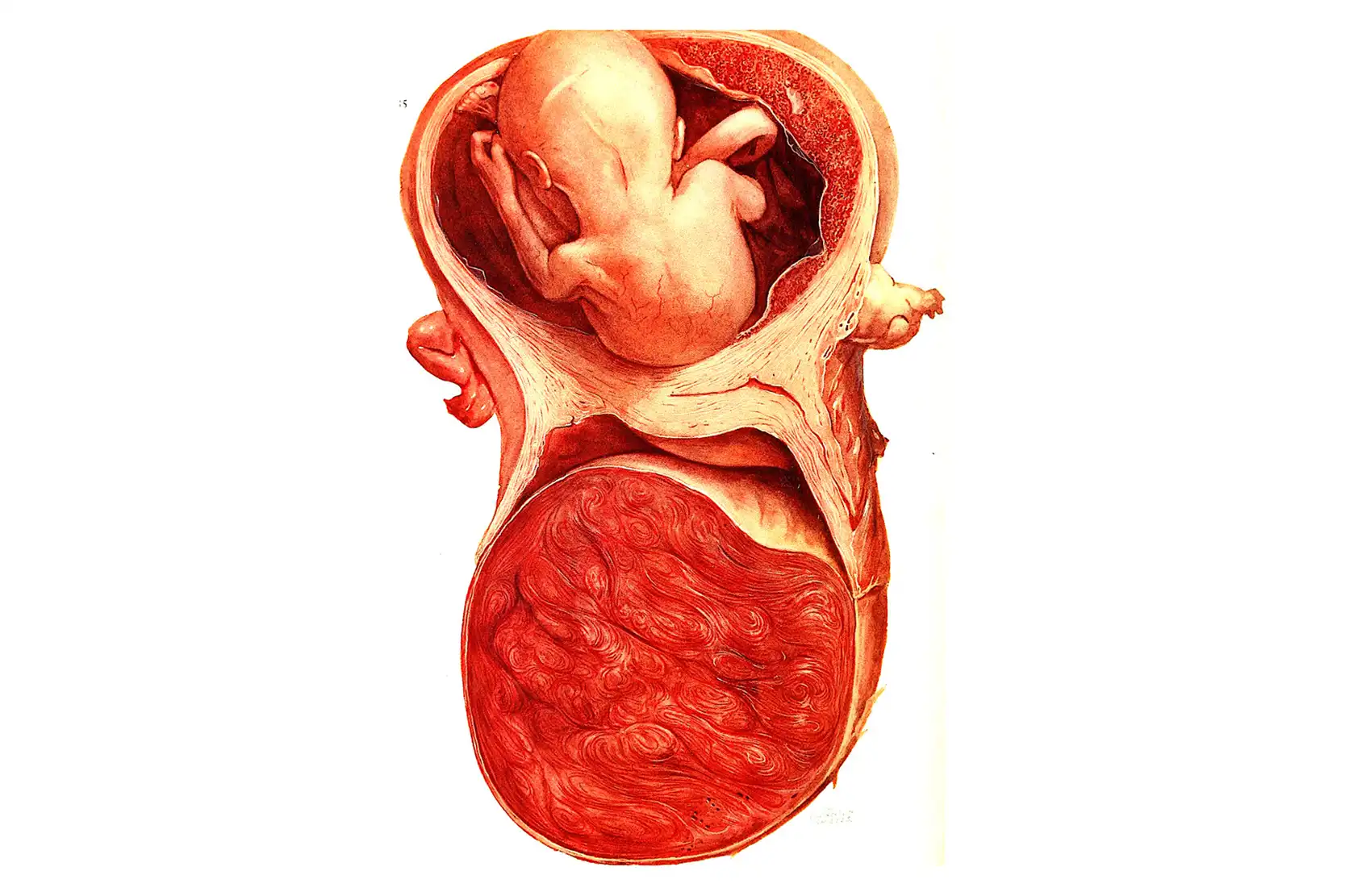
Prenatal Factors: Epilepsy can sometimes be linked to events that occur during fetal development. These may include prenatal exposure to toxins, infections, or complications during pregnancy and childbirth.
Neurological Disorders: Other neurological disorders, such as Alzheimer’s disease, multiple sclerosis, or neurodegenerative disorders, can increase the risk of epilepsy.
Infections: Certain infections affecting the brain, such as cysticercosis or toxoplasmosis, can lead to epilepsy.
Metabolic Disorders: Imbalances in electrolytes, blood sugar levels, or other metabolic disturbances can trigger seizures and contribute to epilepsy.
Autoimmune Disorders: In rare cases, autoimmune disorders that affect the brain’s functioning, such as autoimmune encephalitis, may lead to epilepsy.
Developmental Disorders: Some developmental disorders, such as autism spectrum disorder or intellectual disabilities, may be associated with an increased risk of epilepsy.

Diagnosis of Epilepsy:
Diagnosing epilepsy involves a thorough evaluation of a person’s medical history, symptoms, and diagnostic tests. The process typically includes the following steps.
Medical History: The healthcare provider will begin by taking a detailed medical history, including information about the individual’s symptoms, any previous seizures or seizure-like episodes, family history of epilepsy or other neurological conditions, as well as any potential triggers or risk factors.
Physical Examination: A physical examination will be conducted to assess neurological function, looking for any signs or symptoms suggestive of epilepsy or other neurological disorders.
Electroencephalogram (EEG): EEG is a key diagnostic test for epilepsy. It records the brain’s electrical activity using electrodes attached to the scalp. Abnormal patterns of electrical activity, known as epileptiform discharges, can indicate the presence of epilepsy.
Imaging Studies: Imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be performed to identify any structural abnormalities or lesions in the brain that could be causing seizures.
Blood Tests: Blood tests may be conducted to check for underlying medical conditions, such as infections, metabolic disorders, or genetic factors that may contribute to epilepsy.
Video EEG Monitoring: In some cases, prolonged video EEG monitoring may be necessary to capture and record seizure activity over an extended period. This can help confirm the diagnosis of epilepsy and provide valuable information about the type and frequency of seizures.
Neuropsychological Testing: Neuropsychological testing may be recommended to assess cognitive function, memory, and other aspects of brain function that may be affected by epilepsy.
Diagnostic Criteria: Diagnosis of epilepsy is typically based on specific criteria established by medical organizations, such as the International League Against Epilepsy (ILAE). These criteria take into account the frequency, type, and characteristics of seizures, as well as the results of diagnostic tests.
Specialists Doctor: Diagnosis and management of epilepsy often involve collaboration between different healthcare specialists, including neurologists, epileptologists, neurosurgeons, and other members of the healthcare team.
Treatment Options for Epilepsy:
Epilepsy treatment aims to control seizures and minimize their impact on daily life. The choice of treatment depends on various factors, including the type of seizures, their frequency and severity, the individual’s overall health, and their preferences. Common treatment options for epilepsy include.
Medications (Antiepileptic Drugs, AEDs): Antiepileptic drugs are the most common and effective treatment for epilepsy. They work by stabilizing electrical activity in the brain and reducing the likelihood of seizures. There are many different types of AEDs available, and the choice of medication depends on factors such as seizure type, age, gender, and potential side effects. It’s essential for individuals with epilepsy to take their medications consistently as prescribed by their healthcare provider to achieve optimal seizure control.
Surgery: Surgery may be considered for individuals with epilepsy who do not respond to medications or have seizures originating from a specific, identifiable area of the brain. The most common type of epilepsy surgery is resective surgery, where the part of the brain causing seizures is removed or disconnected (such as a temporal lobectomy for temporal lobe epilepsy). Other surgical procedures, such as corpus callosotomy or vagus nerve stimulation (VNS), may be considered for certain types of epilepsy or when resective surgery is not feasible.
Dietary Therapies: Dietary therapies, such as the ketogenic diet or modified Atkins diet, may be recommended for individuals with epilepsy, particularly children or those who do not respond well to medications. These diets are high in fats and low in carbohydrates and can help control seizures in some people by altering the brain’s metabolism.
Lifestyle Modifications: Certain lifestyle changes may help manage epilepsy and reduce the risk of seizures. These may include getting enough sleep, managing stress, avoiding alcohol and recreational drugs, and maintaining a healthy diet and regular exercise routine.
Vagus Nerve Stimulation (VNS): Vagus nerve stimulation is a treatment option for individuals with epilepsy who do not respond to medications or are not candidates for surgery. It involves implanting a device that delivers electrical impulses to the vagus nerve, which can help reduce the frequency and severity of seizures.
Biofeedback and Neurofeedback: Biofeedback and neurofeedback techniques may be used as adjunctive therapies for epilepsy management. These techniques aim to teach individuals how to control physiological processes, such as heart rate and brainwave patterns, through relaxation and self-regulation techniques.
Clinical Trials and Emerging Therapies: Individuals with refractory epilepsy or those seeking alternative treatments may consider participating in clinical trials investigating new medications, devices, or therapies for epilepsy management.
Living with Epilepsy:
Living with epilepsy involves managing the condition on a day-to-day basis while striving to maintain a fulfilling and active lifestyle. Here are some key aspects to consider for individuals living with epilepsy.
Managing Seizures: Understanding and recognizing seizure triggers, warning signs, and aura symptoms can help individuals better manage their seizures. Following medication schedules consistently and communicating any changes in seizure frequency or severity to healthcare providers are crucial steps in seizure management.
Lifestyle Adjustments: Making lifestyle adjustments, such as ensuring adequate sleep, managing stress, avoiding alcohol and recreational drugs, and maintaining a healthy diet and regular exercise routine, can help reduce the risk of seizures and improve overall well-being. Individuals with epilepsy should also consider safety precautions, such as avoiding activities that pose a risk of injury during seizures, swimming with a buddy, and wearing medical alert identification.
Support Networks: Building a strong support network of family, friends, and healthcare professionals can provide emotional support, practical assistance, and valuable resources for managing epilepsy. Support groups and online communities can also offer opportunities for connecting with others who understand the challenges of living with epilepsy and sharing experiences and coping strategies.
Education and Advocacy: Educating oneself about epilepsy, including its causes, symptoms, treatment options, and rights, is essential for effective self-advocacy and empowerment. Advocating for epilepsy awareness, destigmatization, and access to healthcare resources can help improve understanding and support within the community and society at large.
Driving and Employment: Depending on local regulations and individual circumstances, individuals with epilepsy may need to adhere to specific guidelines regarding driving privileges and employment restrictions. It’s important to understand and comply with relevant laws and regulations while exploring opportunities for meaningful employment and career advancement.
Emotional Well-being: Coping with epilepsy may involve navigating various emotional challenges, including fear, anxiety, depression, and social isolation. Seeking professional counseling or therapy, practicing stress management techniques, engaging in hobbies and activities that bring joy, and maintaining open communication with loved ones can promote emotional resilience and well-being.
Regular Healthcare Monitoring: Regular follow-up appointments with healthcare providers are essential for monitoring treatment effectiveness, managing medication side effects, and addressing any concerns or changes in seizure control. Individuals with epilepsy should also ensure access to emergency medical care and have a seizure action plan in place for themselves and their caregivers.
Raising Awareness for Epilepsy:
Raising awareness for epilepsy is essential to increase understanding, reduce stigma, and promote support for individuals living with the condition. Here are some effective strategies for raising awareness.
Education Campaigns: Organize educational campaigns in schools, workplaces, and community centers to raise awareness about epilepsy, its causes, symptoms, and treatment options. Distribute informational materials, such as brochures, posters, and fact sheets, to provide accurate information and dispel myths and misconceptions about epilepsy.
Social Media Campaigns: Utilize social media platforms to share personal stories, educational resources, and awareness messages about epilepsy. Encourage individuals to share their experiences and insights using dedicated hashtags and participate in online discussions to amplify the reach of awareness efforts.
Events and Fundraisers: Organize events, such as walks, runs, bike rides, or charity galas, to raise funds for epilepsy research, support services, and advocacy initiatives. Host educational seminars, workshops, or panel discussions featuring healthcare professionals, advocates, and individuals living with epilepsy to engage the community and raise awareness.
Partnerships and Collaborations: Collaborate with local organizations, schools, businesses, and healthcare providers to organize awareness events, workshops, and outreach activities. Partner with media outlets, influencers, and celebrities to raise the profile of epilepsy awareness initiatives and reach a broader audience.
Purple Day: Participate in Purple Day, an international epilepsy awareness day held annually on March 26th. Wear purple clothing, accessories, or ribbons, and organize events or activities to raise awareness and support for epilepsy.
Community Engagement: Engage with local communities through outreach events, presentations, and workshops to provide information and support to individuals affected by epilepsy and their families. Foster partnerships with community organizations, religious institutions, and cultural groups to reach diverse populations and raise awareness about epilepsy within different communities.
FAQs about Epilepsy or Seizures:
A1: Generalized seizures and focal seizures are the two main types of seizures associated with epilepsy.
A2: While epilepsy cannot always be cured, it can often be managed effectively with medications and other treatment options.
A3: Diagnosis typically involves a medical history, physical examination, and tests such as EEG and imaging studies.
A4: Genetic factors can play a role in some cases of epilepsy, but not all cases are inherited.
A5: Providing understanding, assistance during seizures, and encouraging them to follow their treatment plan can be supportive.
-Please remember, to always consult with healthcare professionals or Doctors for personalized advice related to medical conditions.
Conclusion:
Epilepsy is a neurological disorder characterized by recurrent seizures, affecting millions of people worldwide. While managing epilepsy can be challenging, proper diagnosis, treatment, and support can significantly improve the quality of life for individuals with epilepsy.