HEALTH BLOG
Hypertrophic Cardiomyopathy or HCM: Causes, Symptoms, Treatment
-
Rahul Priydarss
Discover everything you need to know about Hypertrophic Cardiomyopathy (HCM) in this comprehensive guide. From understanding its causes and symptoms to exploring diagnosis methods and treatment options, this article covers it all. Learn about the latest advancements in HCM research and gain insights into managing this complex cardiovascular condition. Whether you’re seeking information for yourself or a loved one, this article provides valuable insights to help navigate HCM effectively. Dive deep into the world of HCM and empower yourself with knowledge for better heart health.
Introduction to Hypertrophic Cardiomyopathy (HCM):
Hypertrophic Cardiomyopathy (HCM) is a cardiovascular condition characterized by the thickening of the heart muscle, particularly in the left ventricle. This thickening, also known as hypertrophy, makes it harder for the heart to pump blood effectively. HCM is considered the most common genetic cardiovascular disorder and can affect individuals of all ages, from infants to older adults.
This condition can lead to various symptoms and complications, making it essential for individuals with HCM to receive timely diagnosis and appropriate management. In this article, we will delve deeper into understanding the causes, symptoms, diagnosis, treatment options, and lifestyle modifications associated with HCM, as well as explore the perspectives of patients living with this condition and discuss ongoing research efforts in HCM management.
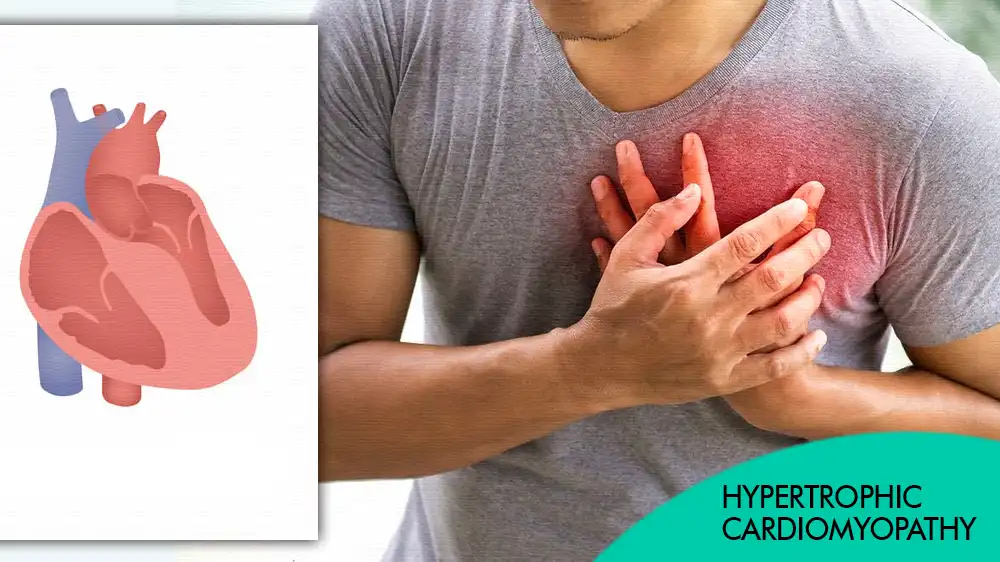
Table of Contents
What is Hypertrophic Cardiomyopathy or HCM:
Hypertrophic Cardiomyopathy (HCM) is a heart condition characterized by the thickening of the heart muscle, particularly the walls of the left ventricle. This thickening can make it harder for the heart to pump blood effectively. HCM is a genetic condition, meaning it’s passed down through families, although it can also occur spontaneously. It’s one of the most common genetic cardiovascular disorders, affecting people of all ages.
Causes of Hypertrophic Cardiomyopathy (HCM):
Hypertrophic Cardiomyopathy (HCM) arises from various factors, predominantly genetic mutations that affect the heart’s structure and function. Here’s a breakdown of the primary causes.
Genetic Mutations: HCM is largely attributed to genetic anomalies, particularly mutations in genes responsible for heart muscle proteins. These mutations disrupt the normal contraction of the heart muscle, leading to thickening of the heart walls. Common genes associated with HCM include MYH7, MYBPC3, TNNT2, and TNNI3, which play vital roles in cardiac function.
Familial Inheritance: HCM often exhibits familial inheritance patterns, meaning it runs in families. It follows an autosomal dominant inheritance pattern, where a single copy of the mutated gene from either parent is sufficient to cause the condition in offspring. Individuals with a family history of HCM are at a higher risk of developing the condition.
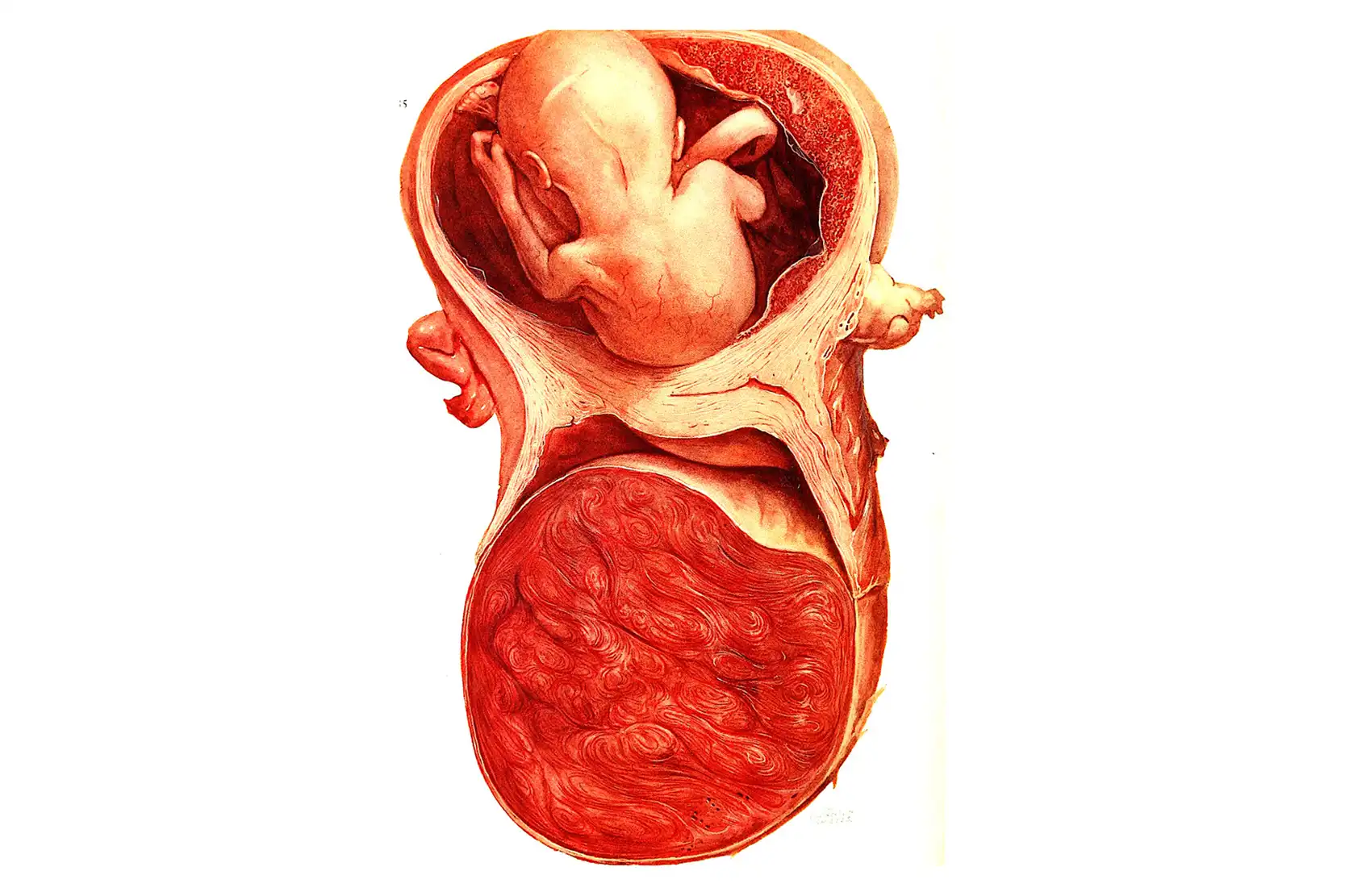
Spontaneous Mutations: In some cases, HCM can occur due to spontaneous mutations in genes, even in the absence of a family history of the condition. These mutations may arise during fetal development or later in life and can lead to the development of HCM without any familial predisposition.
Symptoms of Hypertrophic Cardiomyopathy (HCM):
Hypertrophic Cardiomyopathy (HCM) manifests with a variety of symptoms, which can range from mild to severe. Here are the common symptoms associated with HCM.
Chest Pain (Angina): Many individuals with HCM experience chest pain, particularly during physical activity or exertion. This chest pain, known as angina, occurs due to reduced blood flow to the heart muscle.
Shortness of Breath (Dyspnea): HCM can lead to shortness of breath, especially during physical exertion or when lying flat. The heart’s inability to pump blood effectively results in inadequate oxygen delivery to the body, causing breathlessness.
Fainting Spells (Syncope): Some HCM patients may experience fainting spells or syncope, which occur due to a sudden drop in blood pressure and inadequate blood flow to the brain. Syncope episodes can occur during physical activity or even at rest and may be a sign of underlying cardiac issues.
Fatigue: Fatigue and weakness are common symptoms of HCM, often due to the heart’s decreased ability to pump blood efficiently. Individuals with HCM may feel tired even after minimal exertion or activity.
Heart Palpitations: Palpitations, or irregular heartbeats, are frequently reported by individuals with HCM. These palpitations may feel like the heart is fluttering, pounding, or skipping beats and can be alarming for the individual experiencing them.
Dizziness or Lightheadedness: HCM can cause dizziness or lightheadedness, particularly when standing up quickly or after exertion. These symptoms may occur due to inadequate blood flow to the brain resulting from the heart’s impaired pumping function.
Swelling (Edema): In advanced cases of HCM, fluid retention and swelling, known as edema, may develop in the legs, ankles, feet, or abdomen. Edema occurs when the heart’s reduced pumping capacity leads to fluid accumulation in the body’s tissues.
Arrhythmias: HCM patients are at an increased risk of developing abnormal heart rhythms or arrhythmias. These arrhythmias can cause palpitations, dizziness, fainting, or even sudden cardiac arrest in severe cases.

Diagnosing Hypertrophic Cardiomyopathy (HCM):
Diagnosing Hypertrophic Cardiomyopathy (HCM) involves a combination of medical history assessment, physical examination, imaging tests, and genetic testing. Here’s how healthcare professionals typically diagnose HCM.
Medical History and Physical Examination: The process begins with a thorough review of the patient’s medical history, including any family history of heart conditions. A comprehensive physical examination is conducted to assess for signs of HCM, such as abnormal heart sounds (murmurs) or evidence of heart failure.
Electrocardiogram (ECG or EKG): An electrocardiogram is a non-invasive test that measures the heart’s electrical activity. In individuals with HCM, an ECG may reveal characteristic abnormalities, such as abnormal heart rhythms (arrhythmias) or changes indicative of left ventricular hypertrophy.
Echocardiogram: An echocardiogram uses sound waves to create images of the heart’s structure and function. This imaging test allows healthcare providers to visualize the thickness of the heart muscle, assess blood flow through the heart chambers, and detect any abnormalities in heart valve function. Echocardiography is considered the primary imaging modality for diagnosing HCM and monitoring disease progression.
Cardiac MRI (Magnetic Resonance Imaging): In some cases, cardiac MRI may be recommended to provide more detailed imaging of the heart and assess the extent of hypertrophy. Cardiac MRI can also help identify areas of scar tissue or fibrosis within the heart muscle, which may indicate a higher risk of complications.
Genetic Testing: Genetic testing may be recommended for individuals with suspected or confirmed HCM, particularly those with a family history of the condition. Genetic testing can identify specific mutations in genes associated with HCM, helping to confirm the diagnosis and assess the risk of HCM in family members.
Exercise Stress Testing: Exercise stress testing may be performed to evaluate the heart’s response to physical activity and assess for exercise-induced symptoms, such as chest pain or abnormal heart rhythms. This test can help determine the severity of symptoms and guide treatment recommendations.
Holter Monitoring: Holter monitoring involves wearing a portable device that continuously records the heart’s electrical activity throughout 24 to 48 hours. Holter monitoring may be used to detect arrhythmias or abnormal heart rhythms that occur intermittently and may not be captured during a standard ECG.
Treatment of Hypertrophic Cardiomyopathy (HCM):
The treatment of Hypertrophic Cardiomyopathy (HCM) aims to alleviate symptoms, prevent complications, and improve quality of life. The approach to treatment may vary depending on the severity of symptoms and the presence of specific risk factors. Here are the main treatment options for HCM.
Medications: Medications are often prescribed to manage symptoms and reduce the risk of complications in individuals with HCM. Beta-blockers, calcium channel blockers, and antiarrhythmic drugs may be used to control heart rate, rhythm, and blood pressure. Medications such as diuretics may be prescribed to reduce fluid retention and alleviate symptoms of heart failure.
Implantable Cardioverter-Defibrillator (ICD): In individuals at high risk of sudden cardiac death due to life-threatening arrhythmias, an implantable cardioverter-defibrillator (ICD) may be recommended. An ICD is a small device implanted under the skin that continuously monitors the heart’s rhythm and delivers electric shocks to restore normal rhythm if a dangerous arrhythmia occurs.
Septal Myectomy: For individuals with severe symptoms that are not controlled with medication, surgical intervention may be necessary. Septal myectomy is a surgical procedure performed to remove a portion of the thickened heart muscle (septum) that obstructs blood flow out of the heart. This procedure aims to improve blood flow and alleviate symptoms of heart failure and exercise intolerance.
Alcohol Septal Ablation: Alcohol septal ablation is a minimally invasive procedure used to treat HCM by injecting alcohol into the artery that supplies blood to the thickened heart muscle. This procedure causes selective damage to the overgrown heart muscle, reducing obstruction and improving blood flow.
Lifestyle Modifications: Lifestyle modifications play a crucial role in managing HCM and reducing the risk of complications. Individuals with HCM are advised to avoid strenuous physical activity and competitive sports, as intense exercise can exacerbate symptoms and increase the risk of arrhythmias. Maintaining a healthy diet, managing stress, avoiding tobacco and excessive alcohol consumption, and maintaining a healthy weight are also important for overall heart health.
Regular Monitoring and Follow-Up: Regular medical check-ups and monitoring are essential for individuals with HCM to assess disease progression, adjust treatment as needed, and address any new symptoms or concerns. Monitoring may include regular echocardiograms, ECGs, and Holter monitoring to evaluate heart function and detect any changes in the condition.
Research and Future Directions for HCM:
Hypertrophic cardiomyopathy (HCM) research is bustling with activity, particularly focused on improved diagnosis, targeted therapies, and risk stratification. Here’s a breakdown of the latest advancements and upcoming directions.
Diagnosis and Risk Stratification:
Early Identification: A major focus is pinpointing individuals with a genetic predisposition (genotype-positive) before symptoms develop (phenotype-negative). Early detection allows intervention before the heart muscle stiffens and complications arise.
Risk Factors: Research is ongoing to refine risk assessment for sudden cardiac death, a major concern in HCM. This might involve identifying specific genetic mutations or physiological markers that predict worse outcomes.
Treatment Advancements:
Myosin Inhibition: Mavacamten, a first-in-class drug, reduces excessive heart muscle contraction and has shown promise in improving symptoms and quality of life in patients with obstructive HCM.
Gene Therapy: The future might hold gene editing techniques to address the underlying genetic mutations causing HCM. This is a nascent field with significant potential but requires further research for safe and effective application.
FAQs about HCM:
A1: Yes, HCM often runs in families and can be inherited from one or both parents.
A2: While there is no cure for HCM, treatment can help manage symptoms and improve quality of life.
A3: Long-term complications of HCM may include heart failure, arrhythmias, and sudden cardiac death.
A4: Yes, genetic testing can identify individuals at risk of developing HCM before symptoms appear.
A5: Lifestyle modifications such as avoiding vigorous exercise, monitoring fluid intake, and regular medical check-ups can help manage symptoms and reduce the risk of complications.

-Please remember, to always consult with healthcare professionals or Doctors for personalised advice related to medical conditions.
Conclusion:
In conclusion, Hypertrophic Cardiomyopathy (HCM) is a complex cardiovascular condition characterized by the thickening of the heart muscle, particularly in the left ventricle. This thickening can lead to a range of symptoms, including chest pain, shortness of breath, fainting spells, and fatigue, among others.