Whether you’re newly diagnosed or managing flare-ups, this resource offers everything you need to know to live better with ulcerative colitis. Discover the best ways to reduce inflammation, improve gut health, and avoid triggers through personalized care and evidence-based treatment strategies.
Introduction to Ulcerative colitis:
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers in the innermost lining of your large intestine (colon) and rectum. If you’ve ever struggled with ongoing abdominal pain, frequent trips to the bathroom, or bloody stools, you’re not alone and you might be dealing with ulcerative colitis (UC). As someone who’s navigated this journey personally and professionally, I understand how life-altering it can be. This guide isn’t just from a medical standpoint it’s shaped by real experience, thorough research, and what actually helps people live better with UC.
Ulcerative colitis is more than just a “gut issue” it’s an autoimmune condition that can disrupt your daily life, affect your mood, and make eating feel like a risk. But the good news is: with the right diagnosis, personalized treatment, and lifestyle adjustments, people with UC can live active, fulfilling lives. Let’s walk through everything you need to know from symptoms to treatments, causes to diets so you’re empowered to take control of your health.
No, but it can be managed effectively through medication, diet, and lifestyle changes to reduce flare-ups and improve quality of life.
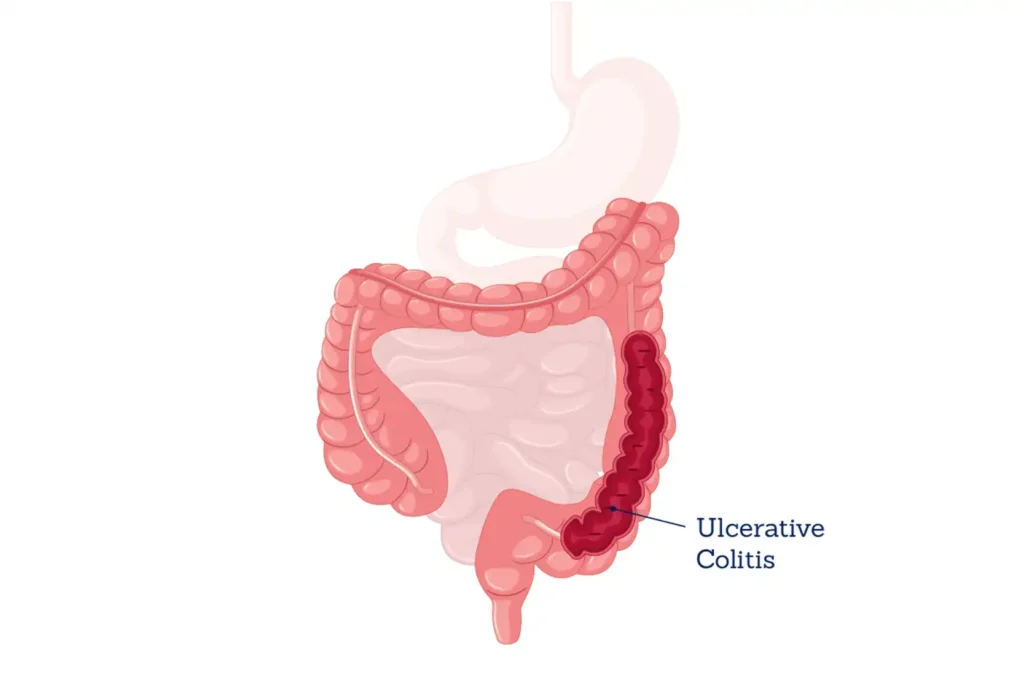
What Is Ulcerative Colitis:
Ulcerative colitis is a type of inflammatory bowel disease (IBD), alongside Crohn’s disease. It specifically affects the large intestine (colon) and rectum, causing chronic inflammation and tiny sores or ulcers on the lining of the colon. These ulcers can bleed, produce pus, and make digestion painful and inefficient.
This condition is considered autoimmune your immune system mistakenly attacks healthy cells in the colon. The result is ongoing inflammation that flares up in cycles. Some people may go weeks, months, or even years without symptoms, while others experience frequent flare-ups. It’s unpredictable, which is why understanding UC deeply is key to managing it effectively.
What Causes Ulcerative Colitis:
The exact cause of ulcerative colitis isn’t known, but it’s believed to be a mix of genetic, environmental, and immune system factors. If you have a family member with UC, your risk is higher. However, lifestyle choices and environmental exposures may also trigger symptoms in people who are genetically predisposed.
An overactive immune response is central to UC. When your immune system encounters a threat (like bacteria), it responds with inflammation. In UC, that response continues even when the threat is gone, attacking healthy cells in the colon lining. Some theories also suggest that certain gut bacteria, stress, and a Western-style diet may contribute to triggering the disease.
Common Symptoms of Ulcerative Colitis:
Symptoms of UC can range from mild to severe and may change over time. The most common symptoms include. Symptoms typically develop gradually rather than all at once. It’s also common to experience periods of remission where symptoms disappear entirely followed by flare-ups.
- Abdominal pain and cramping, often in the lower abdomen.
- Chronic diarrhea, often with blood or mucus.
- Urgency to have bowel movements, even when the colon is empty.
- Fatigue, due to inflammation and nutrient malabsorption.
- Weight loss and appetite loss.
- In some cases, fever and joint pain may also occur.
How Ulcerative Colitis Is Diagnosed:
Getting a diagnosis starts with a detailed history and physical examination. Your doctor will likely ask about your symptoms, family history, and bowel habits. Then, several tests help confirm the diagnosis. A confirmed diagnosis often requires ruling out Crohn’s disease, irritable bowel syndrome (IBS), infections, or colon cancer.
- Colonoscopy or sigmoidoscopy to visualize inflammation and collect biopsies.
- Stool tests to rule out infections or parasites.
- Blood tests to check for anemia or elevated inflammatory markers like CRP or ESR.
- Imaging tests like CT or MRI may be used for a better view of the colon.
Treatment Options for Ulcerative Colitis:
Treatment aims to reduce inflammation, manage symptoms, and maintain long-term remission. The approach usually includes medications, lifestyle changes, and in severe cases, surgery.
- Medications:
- Aminosalicylates (5-ASAs) like mesalamine help reduce inflammation.
- Corticosteroids are used short-term for flare-ups.
- Immunosuppressants like azathioprine help keep the immune system in check.
- Biologics such as infliximab target specific proteins in the immune response.
- JAK inhibitors are newer and effective in certain cases.
- Surgery: In severe or unresponsive cases, a proctocolectomy (removal of colon and rectum) may be necessary, sometimes followed by a J-pouch surgery.
- Supportive Care: Antidiarrheals, pain relievers, and iron supplements may be prescribed.
Ulcerative Colitis Diet and Nutrition Tips:
There’s no one-size-fits-all UC diet, but avoiding trigger foods and eating nutrient-dense meals can greatly help manage flare-ups and keep your gut calm. Keeping a food diary is incredibly helpful for tracking what works (and doesn’t) for you.
During flares, opt for:
- Low-fiber, bland foods like white rice, bananas, eggs, and cooked vegetables.
- Hydrating fluids like broths and electrolyte drinks.
During remission, try:
- A balanced diet with lean proteins, healthy fats, and soft veggies.
- Fermented foods (if tolerated) to support gut health.
Avoid:
- High-fat, greasy foods
- Dairy (if lactose intolerant)
- Alcohol, caffeine, and spicy foods
- Carbonated drinks
Lifestyle Tips to Manage Ulcerative Colitis:
Living with UC means adjusting not just your food but your lifestyle. Here are key habits that help. Regular follow-ups with your gastroenterologist and mental health check-ins also go a long way.
- Stress management is crucial. Stress doesn’t cause UC but can trigger flares. Try meditation, yoga, or breathing exercises.
- Stay active low-impact exercises like walking or swimming reduce inflammation and boost energy.
- Quit smoking (especially if you switch from Crohn’s disease), and limit alcohol.
- Get enough sleep, because rest helps heal your gut and balance immune responses.
What’s the Long-Term Outlook for Ulcerative Colitis:
While UC is a chronic condition with no current cure, many people live long, active lives with it. With early diagnosis and consistent treatment, it’s possible to keep the disease under control for years.
Modern medications and improved surgical options have significantly increased quality of life. Regular colonoscopies are essential, as long-standing UC can increase the risk of colon cancer especially after 8–10 years of diagnosis. The key is personalized care and staying proactive with your health management.
FAQ
Most frequent questions and answers
No, but it can be managed effectively through medication, diet, and lifestyle changes to reduce flare-ups and improve quality of life.
While not usually life-threatening, severe complications like colon perforation or toxic megacolon can occur if untreated. Proper care reduces these risks.
Ulcerative colitis doesn’t go away without treatment. It may go into remission, but flares can return. Long-term management is necessary.
Conclusion:
Living with ulcerative colitis can be challenging, but with the right approach, it’s absolutely manageable. From understanding symptoms to making smart dietary and lifestyle choices, staying informed is your best defense. The more you know about ulcerative colitis, the better equipped you’ll be to reduce flare-ups, improve your quality of life, and take control of your health. Always consult with your healthcare provider, stay consistent with treatment, and remember you’re not alone on this journey. Support and solutions are available.