HEALTH BLOG
West Nile Virus: Unveiling the Mystery and Symptoms
-
Rahul Priydarss
Discover a comprehensive guide to West Nile Virus, delving into its origins, symptoms, diagnosis, treatment, and prevention. Unravel the complexities of this infectious enigma, explore its global spread, transmission dynamics, and debunk common myths. Stay informed with recent research insights and severe case studies, equipping yourself to navigate the challenges posed by this elusive pathogen effectively.
Introduction of West Nile Virus:
In the labyrinth of infectious diseases, a spectral presence has silently woven its way through the corridors of history, touching continents and leaving its mark on the human condition. The West Nile virus, named after its birthplace in the verdant West Nile district of Uganda, is a testament to the delicate balance between nature and mankind, a reminder of how a seemingly inconspicuous entity can ripple through the fabric of our lives. Its tale is one of mystery and intrigue, a journey that spans from the secluded shores of the Nile to the bustling cities of the Western world, and it is here that we begin our exploration of this enigmatic virus.

Table of Contents
The Origins of West Nile Virus:
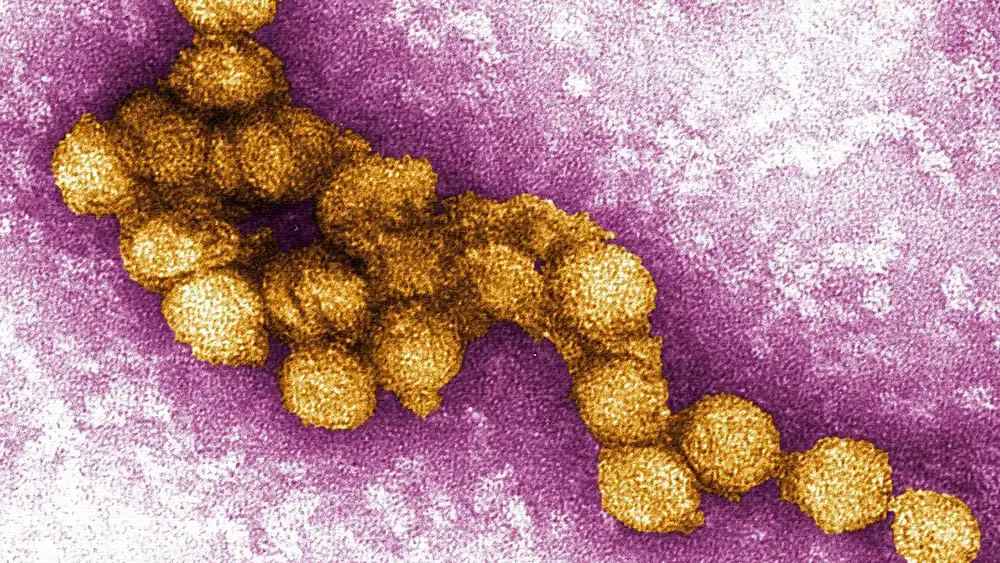
The story of the West Nile virus begins in the heart of Africa, in 1937, when it was first isolated from a feverish woman in Uganda. The virus, belonging to the Flavivirus genus, seemed but a whisper in the grand cacophony of diseases, overshadowed by more notorious afflictions. It lingered in the shadows for decades, with sporadic outbreaks reported across Africa, the Middle East, and parts of Europe. The virus was primarily a concern for birds, its natural hosts, and the occasional equine infection, barely causing a ripple in the broader epidemiological landscape. Yet, like a seed lying dormant, it awaited the right conditions to flourish, to make its presence felt in a world unprepared for its emergence.
The Enigma of West Nile Virus:
West Nile Virus (WNV) is a mosquito-borne pathogen that has perplexed scientists and public health officials since it was first identified in the West Nile district of Uganda in 1937. While it remained relatively obscure for much of the 20th century, the virus gained international notoriety after a significant outbreak in New York City in 1999. Since then, WNV has spread rapidly across the United States, becoming a persistent public health concern.
Understanding the Virus:
WNV is a member of the Flavivirus genus, including other notable viruses like Zika, Dengue, and Yellow Fever. It primarily circulates between birds and mosquitoes, with humans and other mammals serving as incidental hosts. This means that humans and other mammals are not part of the virus’s primary transmission cycle but can become infected if bitten by an infected mosquito.
The majority of WNV infections in humans are asymptomatic. Approximately 80% of those infected will show no symptoms at all. When symptoms do occur, they typically resemble those of the flu: fever, headache, body aches, joint pains, vomiting, diarrhea, or rash. However, about 1 in 150 infected individuals will develop severe illness, which can include encephalitis (inflammation of the brain) or meningitis (inflammation of the membranes surrounding the brain and spinal cord). These severe cases can result in long-term neurological damage or death.
First Identified Cases of West Nile Virus:
West Nile Virus (WNV) was first identified in 1937 in the West Nile district of Uganda, marking the beginning of our understanding of this significant pathogen. Here is a detailed account of the early history of WNV.
Discovery in Uganda:
Initial Identification: The virus was isolated from a woman in the West Nile district who was suffering from a febrile illness. This discovery was part of a broader study on yellow fever conducted by the Rockefeller Foundation’s Virus Research Institute in Entebbe, Uganda. The woman presented with symptoms that included fever, headache, and malaise, which led to the isolation of a previously unknown virus from her blood.
Virus Isolation and Characterization: The isolated virus was named after the region where it was discovered. Researchers initially noted its similarity to other flaviviruses, a group that includes yellow fever and Japanese encephalitis viruses. Subsequent laboratory studies on mice and other animals helped characterize the virus’s pathogenicity and transmission.
Early Outbreaks and Spread:
Initial Spread in Africa and the Middle East: For several decades after its discovery, WNV was primarily confined to Africa and parts of the Middle East. Sporadic outbreaks were reported, often associated with mild febrile illnesses in humans. However, larger outbreaks in Egypt during the 1950s demonstrated the virus’s potential to cause more severe disease, including encephalitis.
Bird and Mosquito Involvement: Research during these early years also identified birds as natural hosts for WNV and mosquitoes as primary vectors. This knowledge was crucial in understanding the virus’s transmission cycle and its potential for widespread impact.
Emergence in Europe and Asia:
Spread to Europe: By the 1960s and 1970s, WNV had spread to parts of Europe, with notable outbreaks occurring in France and Romania. These outbreaks often coincided with periods of increased mosquito activity, underscoring the importance of vector control in managing the virus’s spread.
Introduction to Asia: WNV cases were also reported in Asia, including India and the Soviet Union, further illustrating the virus’s ability to move across continents and affect diverse populations.
Entry into North America:
1999 New York Outbreak: The most significant event in WNV’s history occurred in 1999 when the virus was detected in New York City. This was the first time WNV had been identified in the Western Hemisphere. The outbreak caused significant alarm due to the number of human cases and the high mortality rate among birds, particularly crows.
Rapid Spread Across the US: Following the initial outbreak in New York, WNV spread rapidly across the United States, reaching the West Coast within a few years. By 2004, the virus had been reported in every contiguous state, as well as in Canada and parts of Central and South America.
Transmission and Spread of West Nile Virus:
West Nile Virus (WNV) is primarily transmitted through the bite of infected mosquitoes, particularly species of the Culex genus. Understanding the mechanisms of transmission and the factors influencing the spread of WNV is essential for effective prevention and control efforts. Here’s an overview of how the virus is transmitted and its patterns of spread.
Transmission Cycle:
Mosquito-Bird-Mosquito Cycle: WNV primarily circulates between mosquitoes and birds in what is known as an enzootic cycle. Infected mosquitoes acquire the virus by feeding on infected birds, which serve as reservoir hosts. Once infected, mosquitoes can transmit the virus to other birds when they bite. This perpetuates the cycle of infection among avian populations.
Incidental Transmission to Humans and Other Mammals: While birds are the primary hosts for WNV, humans and other mammals can become infected when bitten by infected mosquitoes. However, humans and other mammals are considered dead-end hosts since they do not produce enough virus in their blood to infect feeding mosquitoes. Nonetheless, these incidental hosts can develop illness if infected, contributing to the public health burden of WNV.
Factors Influencing Spread:
Mosquito Population Dynamics: Mosquito abundance and species distribution play a crucial role in WNV transmission. Factors such as temperature, precipitation, and habitat availability influence mosquito breeding, survival, and activity. Warmer temperatures and stagnant water provide optimal conditions for mosquito proliferation, increasing the risk of WNV transmission.
Bird Migration Patterns: Migratory birds play a significant role in the geographic spread of WNV. Infected birds can carry the virus over long distances during migration, introducing WNV to new regions and contributing to its spread. Certain bird species, such as corvids (e.g., crows and magpies), are particularly susceptible to WNV and can experience high mortality rates during outbreaks.
Human Behavior and Land Use: Human activities, such as urbanization, land development, and changes in land use, can impact mosquito habitats and bird populations, thereby influencing the dynamics of WNV transmission. Urban areas with dense human populations and abundant mosquito breeding sites may experience higher rates of WNV transmission compared to rural areas.
Globalization and Climate Change:
International Travel and Trade: WNV can be transported across continents through the movement of infected humans, animals, or mosquito vectors. International travel and trade facilitate the introduction of WNV to new regions, where it may establish and spread if suitable environmental conditions exist.
Climate Change: Climate variability and change can alter the distribution and abundance of mosquito vectors, as well as the geographic range of WNV. Warmer temperatures and changing precipitation patterns may expand the habitat range of mosquitoes capable of transmitting WNV, potentially leading to the emergence of the virus in regions previously unaffected.
Symptoms of West Nile Virus:
West Nile Virus (WNV) infection can vary widely in severity, with many individuals experiencing no symptoms at all. However, some people may develop mild to severe symptoms, particularly those with compromised immune systems or underlying health conditions. Here are the common symptoms associated with WNV infection.
Fever: Fever is one of the hallmark symptoms of WNV infection. It typically presents as a low-grade fever, ranging from 100.4°F (38°C) to 102.2°F (39°C), although higher fevers may occur in some cases. Fever is the body’s natural response to infection and inflammation caused by the virus.
Headache: Many individuals with WNV infection experience headaches, which can range from mild to severe. Headaches may be persistent and can contribute to feelings of discomfort and malaise.
Body Aches and Joint Pain: Muscle aches (myalgia) and joint pain (arthralgia) are common symptoms of WNV infection, similar to those experienced with the flu. These symptoms may affect multiple muscle groups and joints throughout the body.
Fatigue: Fatigue, or feelings of tiredness and weakness, is frequently reported by individuals with WNV infection. Fatigue may persist for several weeks or even months after other symptoms have resolved.
Nausea and Vomiting: Some people infected with WNV may experience gastrointestinal symptoms such as nausea and vomiting. These symptoms may occur in conjunction with fever and other flu-like symptoms.
Rash: A small percentage of individuals infected with WNV may develop a rash, typically appearing on the trunk of the body but can also occur on other areas such as the arms and legs. The rash may be maculopapular (flat or raised red spots) and sometimes accompanied by itching.
Eye Symptoms: Rarely, WNV infection can cause inflammation of the optic nerve (optic neuritis) or inflammation of the retina (retinitis), leading to vision problems such as blurred vision, eye pain, or sensitivity to light.
Encephalitis: Encephalitis, or inflammation of the brain, is a severe complication of WNV infection that can occur in a subset of cases. Symptoms may include severe headache, confusion, disorientation, tremors, seizures, and coma. Encephalitis can be life-threatening and requires immediate medical attention.
Meningitis: Meningitis, or inflammation of the membranes surrounding the brain and spinal cord, can also occur as a complication of WNV infection. Symptoms of meningitis may include severe headache, neck stiffness, sensitivity to light, nausea, vomiting, and altered mental status.
Muscle Weakness or Paralysis: Severe cases of WNV infection may result in muscle weakness or paralysis, a condition known as acute flaccid paralysis or acute flaccid myelitis. Muscle weakness may affect one or more limbs and can progress rapidly, leading to difficulty moving, walking, or breathing. This condition requires immediate medical attention and may necessitate intensive care and rehabilitation.
Diagnosis of west nile virus:
Diagnosing West Nile Virus (WNV) infection involves a combination of clinical evaluation, laboratory testing, and consideration of epidemiological factors. Here’s an overview of the diagnostic process for WNV.
Clinical Evaluation: Healthcare providers will assess the patient’s symptoms, medical history, and recent travel or exposure to mosquito habitats. Symptoms such as fever, headache, muscle aches, and neurological symptoms may raise suspicion for WNV infection, especially during peak transmission seasons.
Laboratory Testing:
- Serology: Serological tests detect the presence of antibodies produced by the immune system in response to WNV infection. Two types of antibodies are typically measured: Immunoglobulin M (IgM) antibodies, which indicate recent infection, and Immunoglobulin G (IgG) antibodies, which indicate past infection or immunity. Serum or cerebrospinal fluid samples may be tested for WNV-specific antibodies using enzyme-linked immunosorbent assays (ELISA) or other serological methods.
- Molecular Testing: Molecular assays, such as polymerase chain reaction (PCR), can detect viral genetic material (RNA) in blood, cerebrospinal fluid, or other clinical samples. PCR testing is particularly useful for confirming acute WNV infection during the early stages of illness.
Other Tests: In cases of severe neurological illness, additional diagnostic tests may be performed to evaluate brain function, such as computed tomography (CT) or magnetic resonance imaging (MRI) scans, electroencephalography (EEG), and lumbar puncture (spinal tap) to examine cerebrospinal fluid.
Epidemiological Considerations: Epidemiological factors, such as recent travel to areas with known WNV activity or residence in regions experiencing WNV outbreaks, may also inform the diagnostic process. Healthcare providers should consider the patient’s geographical location and the timing of symptoms relative to mosquito season when assessing the likelihood of WNV infection.
Differential Diagnosis: Healthcare providers will also consider other possible causes of similar symptoms, including other viral infections (e.g., influenza, Zika virus), bacterial infections (e.g., meningitis, encephalitis), autoimmune diseases, and non-infectious conditions. Differential diagnosis may require additional testing to rule out alternative diagnoses.
Treatment of West Nile Virus:
Currently, there is no specific antiviral treatment or cure for West Nile Virus (WNV) infection. Treatment primarily focuses on relieving symptoms and providing supportive care for patients, particularly those with severe cases or complications. Here’s an overview of the treatment approach for WNV.
Symptomatic Treatment:
Fever Reduction: Over-the-counter medications such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can help reduce fever and alleviate discomfort associated with WNV infection. These medications should be used according to the manufacturer’s instructions.
Pain Management: Headaches, muscle aches, and joint pain can be managed with analgesic medications such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen. These medications can help relieve pain and discomfort.
Hydration: Encouraging adequate fluid intake, particularly water and electrolyte-rich fluids, is important to prevent dehydration, especially in patients with fever, nausea, or vomiting.
Supportive Care:
Monitoring: Patients with severe symptoms or complications, such as neurological manifestations of WNV infection (e.g., encephalitis, meningitis), may require close monitoring in a hospital setting. Vital signs, neurological status, and hydration levels should be regularly assessed.
Neurological Support: Patients with neurological symptoms may require supportive care to manage complications such as seizures, altered mental status, or muscle weakness. This may involve anticonvulsant medications, sedatives, or mechanical ventilation if respiratory function is compromised.
Prevention of Complications:
Preventing Secondary Infections: Patients with severe WNV infection are at risk of developing secondary bacterial infections, such as pneumonia or urinary tract infections. Prompt diagnosis and treatment of secondary infections are essential to prevent further complications.
Preventing Deep Vein Thrombosis (DVT): Immobilized patients, such as those with severe muscle weakness or paralysis, are at risk of developing deep vein thrombosis (DVT). Measures to prevent DVT, such as leg elevation, compression stockings, and anticoagulant medications, may be necessary.
Rehabilitation:
Physical Therapy: Patients recovering from severe WNV infection, particularly those with muscle weakness or paralysis, may benefit from physical therapy to regain strength, mobility, and function. Physical therapists can design personalized exercise programs to improve muscle strength, balance, and coordination.
Occupational Therapy: Occupational therapy focuses on helping patients relearn activities of daily living and regain independence after neurological complications. Occupational therapists can provide adaptive equipment, techniques, and strategies to facilitate functional independence at home and in the community.
Experimental Treatments:
Antiviral Therapies: Some experimental antiviral therapies, including interferon and ribavirin, have been investigated in clinical studies for the treatment of WNV infection. However, their effectiveness remains uncertain, and further research is needed to evaluate their efficacy and safety in WNV-infected patients.
Prevention of West Nile Virus:
Preventing West Nile Virus (WNV) infection primarily involves minimizing exposure to mosquitoes and reducing the risk of mosquito bites. Here are several preventive measures individuals can take to protect themselves and their communities from WNV.
Mosquito Control:
Eliminate Standing Water: Mosquitoes breed in stagnant water, so it’s essential to eliminate sources of standing water around homes and communities. This includes emptying containers such as flower pots, birdbaths, and clogged gutters where water can accumulate.
Use Mosquito Dunks: For standing water that cannot be drained, such as ponds or rain barrels, use mosquito dunks or larvicides to prevent mosquito breeding. These products contain bacteria that target mosquito larvae and prevent them from developing into adult mosquitoes.
Mosquito Traps: Consider using mosquito traps or other mosquito control devices to reduce mosquito populations in outdoor areas.
Personal Protection Measures:
Use Insect Repellent: Apply EPA-registered insect repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus (OLE) to exposed skin and clothing when outdoors, especially during peak mosquito activity times (dusk and dawn).
Wear Protective Clothing: Wear long-sleeved shirts, long pants, socks, and closed-toe shoes to minimize skin exposure to mosquitoes. Clothing treated with permethrin provides additional protection.
Stay Indoors During Peak Mosquito Activity: Limit outdoor activities during peak mosquito activity times, particularly during dawn and dusk when mosquitoes are most active.
Community Measures:
Mosquito Surveillance and Control Programs: Support community-based mosquito surveillance and control programs. These programs may include larviciding, adulticiding (spraying insecticides to kill adult mosquitoes), and monitoring mosquito populations and disease activity.
Public Education Campaigns: Participate in public education campaigns that promote awareness of WNV and provide information on preventive measures. Encourage community members to take proactive steps to reduce mosquito breeding sites and protect themselves from mosquito bites.
Protection of Vulnerable Populations:
Protective Measures for Infants and Children: Take extra precautions to protect infants and young children from mosquito bites, as they may be more susceptible to severe illness from WNV infection.
Protection for Older Adults and Individuals with Compromised Immune Systems: Older adults and individuals with weakened immune systems are at higher risk of severe complications from WNV infection. Encourage these individuals to take extra precautions to avoid mosquito bites.
Travel Precautions:
Avoid Traveling to Areas with WNV Activity: Check local health advisories and WNV activity reports before traveling to areas where the virus is prevalent. Take appropriate precautions to prevent mosquito bites if travel to affected areas is unavoidable.
Recent Research and Updates on West Nile Virus (2023-2024):
The fight against West Nile Virus (WNV) continues, with ongoing research efforts aimed at understanding the virus better, developing preventative measures, and potentially even treatments. Here’s a glimpse into some key developments from 2023-2024.
Geographic Spread: A significant finding in 2023 was the detection of WNV in a young zoo bird in Rhineland-Palatinate, Germany, an area previously not considered endemic for the virus. This suggests a potential for wider geographic spread than previously thought. Research from the Friedrich-Loeffler-Institut (FLI) in Germany confirmed this notion, highlighting that WNV infections were identified beyond known endemic regions within the country.
Understanding Transmission: Studies are ongoing to elucidate the precise factors influencing WNV transmission dynamics. Climate change is a growing concern, with warmer temperatures potentially leading to increased mosquito populations and a higher risk of outbreaks.
Vaccine Development: While there’s currently no licensed vaccine for WNV, research continues in this area. Several vaccine candidates are under development, with some showing promise in pre-clinical trials. However, further research and human trials are necessary before a WNV vaccine becomes commercially available.
Treatment Advancements: Although there’s no specific antiviral medication for WNV yet, researchers are exploring various treatment options. Some studies are investigating the potential of repurposing existing drugs for WNV treatment, while others are focusing on developing new antiviral therapies.
Early Detection and Surveillance: Early detection of WNV outbreaks is crucial for implementing control measures. Research is ongoing to improve surveillance methods, including developing more sensitive diagnostic tests and better monitoring systems for mosquito populations and potential virus activity.
Public Awareness: Public health agencies continue to emphasize the importance of individual preventive measures like mosquito bite avoidance through the use of repellents and protective clothing. Additionally, educating communities about eliminating mosquito breeding grounds remains a key public health strategy.
Knowledge Gaps and Future Directions: Despite significant progress, there are still gaps in our understanding of WNV. More research is needed to understand the long-term effects of WNV infection, particularly on neurological complications. Additionally, investigating the role of different mosquito species in transmission and exploring the potential for spillover into new animal hosts are crucial areas for further exploration.
Myths of West Nile Virus:
Dispelling myths surrounding West Nile Virus (WNV) is crucial for promoting accurate understanding and effective prevention strategies. Here are some common myths about WNV along with explanations debunking them.
Myth: WNV only affects humans.
Fact: While humans can become infected with WNV through mosquito bites, the virus primarily cycles between mosquitoes and birds. Birds serve as reservoir hosts for WNV, and mosquitoes become infected by feeding on infected birds. Other animals, such as horses and some mammals, can also be infected, but they are considered dead-end hosts and do not contribute significantly to the virus’s transmission cycle.
Myth: All mosquitoes carry West Nile Virus.
Fact: Not all mosquito species are capable of transmitting WNV. The primary vectors responsible for transmitting WNV to humans and other animals belong to the Culex genus, particularly Culex pipiens and Culex quinquefasciatus. Additionally, not all mosquitoes within these species are infected with the virus. Surveillance efforts focus on monitoring mosquito populations and identifying areas with increased WNV activity.
Myth: You can get West Nile Virus from direct contact with infected birds.
Fact: WNV is primarily transmitted through the bite of infected mosquitoes and does not spread directly from birds to humans. However, handling dead birds with bare hands should be avoided as a precautionary measure. Proper disposal methods or reporting dead bird sightings to local health authorities can help in monitoring WNV activity and implementing control measures.
Myth: West Nile Virus is only a concern during the summer months.
Fact: While WNV activity peaks during the warmer months when mosquito populations are highest, the virus can circulate year-round in some regions. In temperate climates, WNV transmission typically occurs from late spring to early fall when mosquito activity is most prevalent. However, sporadic cases or localized outbreaks may occur outside of these periods, especially in areas with mild winters.
Myth: West Nile Virus only affects older adults.
Fact: While older adults and individuals with weakened immune systems are at higher risk of developing severe complications from WNV infection, people of all ages can become infected. Severe cases of WNV, including neuroinvasive disease such as encephalitis or meningitis, can occur in individuals of any age. Taking preventive measures to avoid mosquito bites is important for everyone, regardless of age or health status.
2 Severe Case Studies of West Nile Virus:
Case 1: A Young Man with Encephalitis:
Patient: A 25-year-old previously healthy male presented to the emergency department with a fever of 103°F (39.4°C), severe headache, and confusion. He reported feeling unwell for three days prior, experiencing fatigue, muscle aches, and nausea.
Medical History: No significant past medical history or allergies.
Physical Examination: The patient was lethargic and disoriented. He exhibited neck stiffness and weakness in his left arm.
Investigations: Blood tests were normal except for a slightly elevated white blood cell count. An MRI scan of the brain revealed inflammation in the thalamus, a region deep within the brain responsible for various functions like coordination and sensory perception.
Diagnosis: Based on the clinical presentation, imaging findings, and seasonality (peak WNV season), West Nile virus infection was suspected. A blood test confirmed the diagnosis by detecting specific antibodies against WNV.
Treatment: There is no specific antiviral treatment for WNV. The patient received supportive care, including intravenous fluids, pain medication, and anti-nausea medication. He also underwent physical therapy to address the weakness in his arm.
Outcome: The patient’s condition gradually improved over a week. His fever subsided, and his mental status normalized. He regained most of his strength in his arm, although some residual weakness persisted. He was discharged to a rehabilitation facility for continued physical therapy before returning home.
Discussion: This case highlights the potential for severe neurological complications in young, healthy individuals with WNV infection. While most cases are mild, encephalitis can occur, leading to significant morbidity. Early diagnosis and supportive care are crucial for improving outcomes.
Case 2: Immunocompromised Patient with West Nile Meningitis:
Patient: A 72-year-old male with a history of chronic obstructive pulmonary disease (COPD) and receiving long-term immunosuppressive medication for a recent kidney transplant presented to the hospital with a high fever, severe headache, and stiff neck. He reported feeling unwell for five days, experiencing fatigue, muscle aches, and photophobia (sensitivity to light).
Medical History: COPD, kidney transplant on immunosuppressive medication.
Physical Examination: The patient was febrile and appeared lethargic. He exhibited significant neck stiffness and had difficulty concentrating.
Investigations: Blood tests revealed an elevated white blood cell count. A lumbar puncture (spinal tap) showed elevated levels of white blood cells in the cerebrospinal fluid, indicating inflammation of the meninges. A blood test confirmed WNV infection.
Diagnosis: West Nile virus meningitis. The patient’s immunosuppressed state due to his medication likely contributed to the severity of his illness.
Treatment: The patient received supportive care similar to the previous case but also underwent a course of antiviral medication with some potential activity against flaviviruses, although its effectiveness for WNV is not definitively established. He required additional respiratory support due to underlying COPD complications.
Outcome: The patient’s recovery was slower than the younger patient. While his fever subsided and his mental status improved, he experienced lingering weakness and fatigue. He underwent extensive physical therapy to regain strength and eventually returned home, although with some limitations in his daily activities.
Discussion: This case demonstrates the increased risk of severe WNV infection in immunocompromised individuals. The use of antiviral medication is an ongoing area of research, and its role in managing severe WNV cases requires further investigation.
FAQs about West Nile virus:
A1: The West Nile virus is a mosquito-borne virus that can cause illness in humans and animals, ranging from mild fever to severe neurological diseases.
A2: The primary mode of transmission is through the bite of an infected mosquito. Rarely, it can also be spread through blood transfusions, organ transplants, or from mother to baby during pregnancy, delivery, or breastfeeding.
A3: There is no specific cure for West Nile virus. Treatment focuses on relieving symptoms and providing supportive care for severe cases.
A4: Personal protection measures include using insect repellent, wearing long sleeves and pants, and ensuring living areas are mosquito-proof. Community efforts involve mosquito control programs and public education.
A5: As of now, there is no commercially available vaccine for West Nile virus. Research is ongoing to develop an effective vaccine.
-Please remember, to always consult with healthcare professionals or Doctors for personalised advice related to medical conditions.
Conclusion:
In unraveling the enigma of West Nile Virus, we discover its origins in the heart of Africa and its global spread. Symptoms range from mild flu-like illness to severe neurological complications, highlighting the virus’s complexity. Diagnosis involves clinical evaluation, laboratory testing, and consideration of epidemiological factors. Treatment focuses on supportive care, as there’s no specific antiviral therapy. Prevention relies on mosquito control measures and personal protection strategies. Amid ongoing research and public health efforts, dispelling myths and fostering awareness remain vital in combating this elusive pathogen.